Intro
Discover the causes and symptoms of low blood CO2 levels, also known as respiratory alkalosis, and learn how to manage hyperventilation, breathing techniques, and CO2 deficiency for overall health and wellness.
The human body is a complex system that relies on a delicate balance of various elements to function properly. One of these essential elements is carbon dioxide (CO2), a colorless, odorless gas that plays a crucial role in maintaining the body's acid-base balance. Low blood CO2 levels, also known as respiratory alkalosis, can have significant consequences on the body's overall health. In this article, we will delve into the world of low blood CO2 levels, exploring their causes, symptoms, and effects on the body.
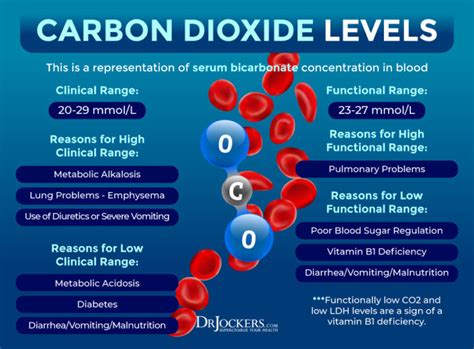
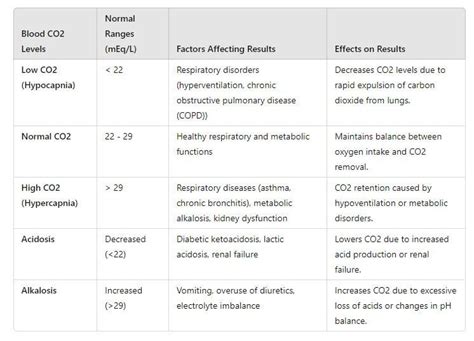
The importance of maintaining optimal CO2 levels in the blood cannot be overstated. CO2 is a byproduct of cellular metabolism, and its levels in the blood are tightly regulated by the respiratory and renal systems. When CO2 levels in the blood drop, it can lead to a range of symptoms, from mild to severe. These symptoms can be debilitating and affect an individual's quality of life. Therefore, it is essential to understand the causes and consequences of low blood CO2 levels to take preventive measures and seek medical attention when necessary.
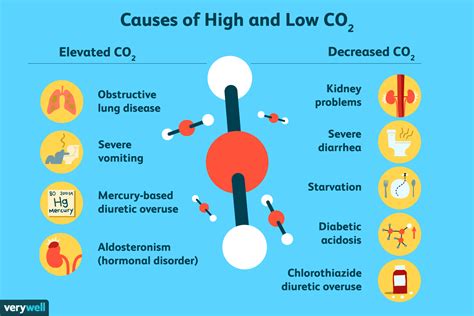
The body's CO2 levels are influenced by various factors, including respiratory rate, depth of breathing, and metabolic rate. When the body's CO2 levels drop, it can be due to hyperventilation, where an individual breathes too quickly or deeply, expelling more CO2 than necessary. This can occur during periods of stress, anxiety, or panic attacks. Other causes of low blood CO2 levels include high-altitude environments, where the air pressure is lower, and certain medical conditions, such as asthma or chronic obstructive pulmonary disease (COPD). Understanding these causes is crucial in addressing low blood CO2 levels and preventing their consequences.
What are Low Blood CO2 Levels?
Causes of Low Blood CO2 Levels
The causes of low blood CO2 levels can be divided into two main categories: respiratory and non-respiratory. Respiratory causes include hyperventilation, high-altitude environments, and certain medical conditions, such as asthma or COPD. Non-respiratory causes include metabolic disorders, such as diabetic ketoacidosis, and certain medications, such as diuretics. Understanding these causes is crucial in addressing low blood CO2 levels and preventing their consequences.Symptoms of Low Blood CO2 Levels
Effects of Low Blood CO2 Levels on the Body
Low blood CO2 levels can have significant effects on the body's overall health. These effects include: * Respiratory problems: Low CO2 levels can lead to respiratory failure, which can be life-threatening. * Cardiovascular problems: Low CO2 levels can lead to cardiac arrhythmias, which can increase the risk of heart attack or stroke. * Neurological problems: Low CO2 levels can lead to seizures, coma, or death. * Metabolic problems: Low CO2 levels can lead to metabolic disorders, such as diabetic ketoacidosis.Treatment and Prevention of Low Blood CO2 Levels

Diagnosis of Low Blood CO2 Levels
Diagnosis of low blood CO2 levels involves a range of tests, including: * Blood gas analysis: This test measures the levels of CO2, oxygen, and other gases in the blood. * Electrolyte panel: This test measures the levels of electrolytes, such as sodium, potassium, and chloride, in the blood. * Complete blood count (CBC): This test measures the levels of red and white blood cells, platelets, and hemoglobin in the blood. * Imaging studies: These studies, such as X-rays or computed tomography (CT) scans, may be used to rule out underlying medical conditions.Complications of Low Blood CO2 Levels
Management of Low Blood CO2 Levels
Management of low blood CO2 levels involves a range of strategies, including: * Breathing exercises: These exercises can help reduce stress and anxiety, which can contribute to hyperventilation. * Relaxation techniques: These techniques, such as meditation or yoga, can help reduce stress and anxiety. * Medication: In some cases, medication may be necessary to address underlying medical conditions. * Supplemental oxygen: In cases of high-altitude environments, supplemental oxygen may be necessary to increase oxygen levels in the blood.Conclusion and Future Directions
Final Thoughts
Low blood CO2 levels are a complex medical condition that requires a comprehensive approach to management. By understanding the causes, symptoms, and effects of low blood CO2 levels, individuals can take preventive measures to reduce their risk of developing this condition. Additionally, healthcare professionals can provide effective treatment and management strategies to address low blood CO2 levels and prevent their complications.What are the symptoms of low blood CO2 levels?
+The symptoms of low blood CO2 levels can vary in severity and include dizziness or lightheadedness, headaches, fatigue, muscle cramps, numbness or tingling in the hands and feet, seizures, respiratory failure, coma, and death.
What are the causes of low blood CO2 levels?
+The causes of low blood CO2 levels can be divided into two main categories: respiratory and non-respiratory. Respiratory causes include hyperventilation, high-altitude environments, and certain medical conditions, such as asthma or COPD. Non-respiratory causes include metabolic disorders, such as diabetic ketoacidosis, and certain medications, such as diuretics.
How are low blood CO2 levels diagnosed?
+Diagnosis of low blood CO2 levels involves a range of tests, including blood gas analysis, electrolyte panel, complete blood count (CBC), and imaging studies, such as X-rays or computed tomography (CT) scans.
What are the complications of low blood CO2 levels?
+Complications of low blood CO2 levels can be severe and life-threatening, including respiratory failure, cardiac arrhythmias, seizures, coma, and death.
How are low blood CO2 levels managed?
+Management of low blood CO2 levels involves a range of strategies, including breathing exercises, relaxation techniques, medication, and supplemental oxygen. In some cases, hospitalization may be necessary to address underlying medical conditions.
