Intro
Manage diabetes with 5 expert tips, including diet control, exercise routines, and glucose monitoring, to maintain healthy blood sugar levels and prevent complications like diabetic neuropathy and retinopathy.
Managing diabetes requires a combination of lifestyle changes, medication, and regular monitoring. For individuals living with diabetes, understanding how to manage their condition effectively is crucial for maintaining their health and preventing complications. Diabetes management involves a range of strategies, from diet and exercise to medication and stress management. Here, we'll explore some key tips for diabetics to help them manage their condition and improve their overall well-being.
Effective diabetes management starts with a comprehensive understanding of the condition itself. Diabetes is a chronic health condition that affects how your body turns food into energy. It's primarily characterized by high blood sugar levels, which can lead to a variety of health issues if not properly managed. There are different types of diabetes, including Type 1, Type 2, and gestational diabetes, each with its unique causes and management approaches. Understanding the specific type of diabetes you have and how it affects your body is the first step towards effective management.
For many individuals with diabetes, managing the condition can seem overwhelming. However, with the right strategies and support, it's possible to control blood sugar levels, prevent complications, and lead a healthy, active life. This involves making informed decisions about diet, physical activity, and medication, as well as staying connected with healthcare providers and support networks. By taking a proactive and informed approach to diabetes management, individuals can significantly improve their quality of life and reduce the risk of diabetes-related health issues.
Understanding Diabetes Management

Understanding diabetes management is crucial for individuals living with the condition. It involves a range of activities, from monitoring blood glucose levels and managing medication to making healthy lifestyle choices. Effective management helps prevent complications such as heart disease, kidney damage, and nerve damage, which can significantly impact an individual's quality of life. By working closely with healthcare providers and staying informed about the latest management strategies, individuals with diabetes can better control their condition and reduce the risk of these complications.
Key Components of Diabetes Management
Effective diabetes management includes several key components: - **Monitoring Blood Glucose Levels:** Regular monitoring helps individuals understand how different factors, such as food and physical activity, affect their blood sugar levels. - **Healthy Eating:** Following a balanced diet that is low in sugar, salt, and unhealthy fats can help manage blood sugar levels and maintain a healthy weight. - **Regular Physical Activity:** Exercise can help lower blood sugar levels and improve insulin sensitivity, making it easier to manage diabetes. - **Medication Management:** For many individuals with diabetes, medication is a crucial part of their management plan. This can include insulin therapy or oral medications that help regulate blood sugar levels. - **Stress Management:** High levels of stress can increase blood sugar levels. Engaging in stress-reducing activities, such as yoga or meditation, can help manage stress and improve overall well-being.Healthy Eating for Diabetics
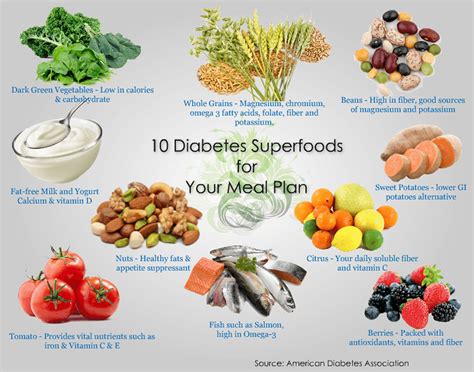
Healthy eating is a cornerstone of diabetes management. It involves choosing foods that are rich in nutrients but low in added sugars, saturated fats, and sodium. A balanced diet can help manage blood sugar levels, maintain a healthy weight, and prevent diabetes-related complications. Key foods for a healthy diabetes diet include whole grains, lean proteins, a variety of colorful vegetables, and fruits. It's also important to stay hydrated by drinking plenty of water and limiting sugary drinks.
Nutritional Planning
Nutritional planning is essential for individuals with diabetes. This involves working with a dietitian or healthcare provider to develop a personalized meal plan that takes into account the individual's nutritional needs, lifestyle, and diabetes management goals. The plan should focus on whole, unprocessed foods and include strategies for managing carbohydrate intake, which directly affects blood sugar levels. Additionally, understanding portion sizes and learning how to read food labels can help individuals make informed choices about their diet.Physical Activity and Diabetes

Regular physical activity is another critical component of diabetes management. Exercise can help lower blood sugar levels, improve insulin sensitivity, and reduce the risk of heart disease and other complications. For individuals with diabetes, it's recommended to engage in at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, per week. Additionally, incorporating strength-training activities, high-intensity interval training, and flexibility exercises can provide additional benefits.
Getting Started with Exercise
Getting started with an exercise program can seem daunting, especially for those who are new to regular physical activity. It's essential to start slowly and gradually increase the intensity and duration of workouts. This might involve beginning with short walks each day and gradually increasing the distance or incorporating strength training exercises into your routine. It's also crucial to listen to your body and rest when needed, as overexertion can lead to injury or burnout.Stress Management for Diabetics

Stress can have a significant impact on blood sugar levels, making stress management an essential part of diabetes care. High levels of stress can lead to increased blood sugar levels, as stress triggers the release of hormones like cortisol and adrenaline, which can cause blood sugar levels to rise. Engaging in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can help manage stress and improve overall well-being.
Practicing Mindfulness
Practicing mindfulness is a powerful way to manage stress and improve diabetes management. Mindfulness involves being present in the moment, focusing on your thoughts, feelings, and sensations without judgment. This can help reduce stress, improve mood, and increase feelings of calm and well-being. Activities like meditation and yoga are excellent ways to cultivate mindfulness and can be adapted to fit any lifestyle or ability level.Medication Management

For many individuals with diabetes, medication is a crucial part of their management plan. This can include insulin therapy for those with Type 1 diabetes or certain individuals with Type 2 diabetes, as well as oral medications that help regulate blood sugar levels. Effective medication management involves taking medications as prescribed, monitoring blood sugar levels regularly, and attending follow-up appointments with healthcare providers to adjust the treatment plan as needed.
Understanding Your Medications
Understanding your medications, including their names, dosages, and potential side effects, is vital for safe and effective medication management. Keeping a medication list and sharing it with all healthcare providers can help prevent drug interactions and ensure that medications are working as intended. It's also important to ask questions and seek clarification if there's any confusion about medication instructions or side effects.Conclusion and Next Steps
Managing diabetes effectively requires a multifaceted approach that includes healthy eating, regular physical activity, stress management, and medication management. By understanding the key components of diabetes care and working closely with healthcare providers, individuals with diabetes can take control of their condition, reduce the risk of complications, and improve their overall quality of life. Whether you're newly diagnosed or have been living with diabetes for years, there's always more to learn and ways to enhance your management plan.
We invite you to share your experiences, ask questions, or seek advice from our community. Your engagement and feedback are invaluable in helping others manage their diabetes journey. Together, we can build a supportive network that fosters education, empowerment, and wellness for all individuals living with diabetes.
What are the primary types of diabetes?
+There are three main types of diabetes: Type 1, Type 2, and gestational diabetes. Type 1 diabetes is an autoimmune condition where the body attacks insulin-producing cells, Type 2 diabetes is characterized by insulin resistance and impaired insulin secretion, and gestational diabetes occurs during pregnancy due to hormonal changes and insulin resistance.
How often should I check my blood sugar levels?
+The frequency of checking blood sugar levels depends on the type of diabetes and the individual's treatment plan. Generally, individuals with Type 1 diabetes and those with Type 2 diabetes who are on insulin therapy may need to check their blood sugar levels several times a day, while those with Type 2 diabetes not on insulin may check less frequently.
Can diet and exercise alone manage diabetes?
+For some individuals with Type 2 diabetes, diet and exercise can be effective in managing the condition, especially in the early stages. However, many people with diabetes will also require medication, including oral medications or insulin therapy, to achieve optimal blood sugar control. It's essential to work with a healthcare provider to determine the best management plan.
