Intro
Discover the Coombs Antiglobulin Test, a diagnostic tool for detecting antibodies, antigens, and immune system disorders, including hemolytic disease and anemia, using indirect and direct methods.
The Coombs test, also known as the antiglobulin test, is a medical laboratory test used to detect the presence of antibodies or complement system factors that are bound to the surface of red blood cells. This test is crucial in the diagnosis and management of various blood-related disorders, including hemolytic disease of the newborn and autoimmune hemolytic anemia. The importance of the Coombs test lies in its ability to identify and differentiate between different types of anemia, allowing healthcare providers to provide targeted treatment and improve patient outcomes.
The Coombs test has been a cornerstone in the field of transfusion medicine for many decades, and its significance extends beyond the diagnosis of anemia. It has also played a critical role in the development of blood banking and transfusion practices, ensuring the safe and compatible transfer of blood components from donors to recipients. The test's impact on patient care is undeniable, and its continued use and refinement have led to improved outcomes and reduced complications in patients with blood-related disorders. As medical research and technology continue to evolve, the Coombs test remains an essential tool in the diagnosis and management of these conditions.
The Coombs test is named after its developer, Robin Coombs, who first introduced the test in the 1940s. Since then, the test has undergone significant improvements and refinements, leading to the development of various modifications and extensions. The test's basic principle involves the use of antiglobulin reagents, which are designed to detect the presence of antibodies or complement factors bound to the surface of red blood cells. The test's sensitivity and specificity have made it an indispensable tool in the diagnosis and management of various blood-related disorders, and its applications continue to expand as new research and technologies emerge.
Introduction to the Coombs Test
Types of Coombs Tests
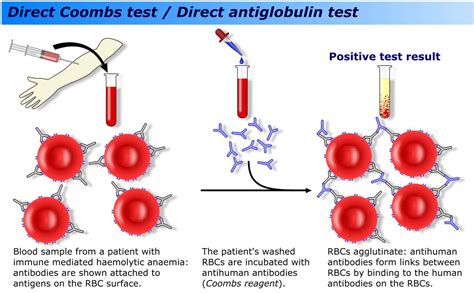
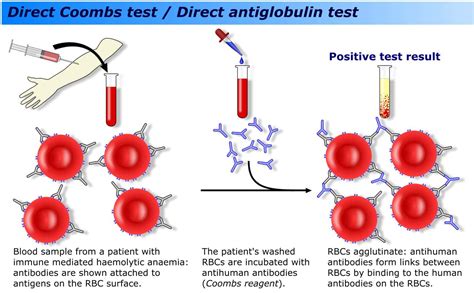
There are two main types of Coombs tests: the direct Coombs test and the indirect Coombs test. The direct Coombs test, also known as the direct antiglobulin test, is used to detect the presence of antibodies or complement factors that are already bound to the surface of red blood cells. This test is typically used to diagnose autoimmune hemolytic anemia and hemolytic disease of the newborn. The indirect Coombs test, also known as the indirect antiglobulin test, is used to detect the presence of antibodies in the serum that are capable of binding to red blood cells. This test is typically used to screen for antibodies prior to blood transfusion.How the Coombs Test Works
Interpreting Coombs Test Results
The results of the Coombs test are typically reported as positive or negative. A positive result indicates the presence of antibodies or complement factors bound to the surface of red blood cells, while a negative result indicates the absence of these factors. The test's sensitivity and specificity are critical in ensuring accurate results, and various factors can influence the test's outcome. These factors include the type and quality of the antiglobulin reagents used, the technique and experience of the laboratory personnel, and the condition and handling of the blood sample.Clinical Applications of the Coombs Test

Limitations and Challenges of the Coombs Test
While the Coombs test is a valuable tool in the diagnosis and management of blood-related disorders, it has several limitations and challenges. The test's sensitivity and specificity can be influenced by various factors, including the type and quality of the antiglobulin reagents used, the technique and experience of the laboratory personnel, and the condition and handling of the blood sample. Additionally, the test may not detect all types of antibodies or complement factors, and false-positive or false-negative results can occur. The Coombs test should be used in conjunction with other diagnostic tests and techniques to ensure accurate results and effective management of blood-related disorders.Future Directions and Emerging Trends
Conclusion and Recommendations
In conclusion, the Coombs test is a valuable tool in the diagnosis and management of blood-related disorders, with a wide range of clinical applications and emerging trends. The test's sensitivity and specificity make it an essential component of transfusion medicine, ensuring the safe and compatible transfer of blood components from donors to recipients. To ensure accurate results and effective management of blood-related disorders, the Coombs test should be used in conjunction with other diagnostic tests and techniques, and healthcare providers should stay up-to-date with the latest developments and refinements in the field.What is the Coombs test used for?
+The Coombs test is used to detect the presence of antibodies or complement system factors that are bound to the surface of red blood cells. It is typically used to diagnose and manage various blood-related disorders, including hemolytic disease of the newborn, autoimmune hemolytic anemia, and alloimmune hemolytic anemia.
How is the Coombs test performed?
+The Coombs test involves the use of antiglobulin reagents, which are designed to detect the presence of antibodies or complement factors bound to the surface of red blood cells. The test's basic principle involves the addition of antiglobulin reagents to a sample of red blood cells, followed by observation for agglutination or hemolysis.
What are the limitations of the Coombs test?
+The Coombs test has several limitations, including the potential for false-positive or false-negative results, and the influence of various factors on the test's sensitivity and specificity. The test should be used in conjunction with other diagnostic tests and techniques to ensure accurate results and effective management of blood-related disorders.
We hope this article has provided you with a comprehensive understanding of the Coombs test and its applications in transfusion medicine. If you have any further questions or would like to learn more about this topic, please do not hesitate to comment or share this article with others. Your feedback and engagement are invaluable in helping us improve our content and provide the best possible information to our readers.
