Intro
Learn about Gb Strep in pregnancy risks, symptoms, and prevention methods, including Group B Strep infection, prenatal testing, and antibiotic treatment to minimize newborn complications and ensure a healthy delivery.
Pregnancy is a unique and delicate period in a woman's life, filled with excitement, anticipation, and a multitude of physiological changes. Among the various health considerations during pregnancy, one critical aspect is the presence of Group B Streptococcus (GBS), commonly referred to as GBS. This bacterium is typically found in the digestive and lower genital tracts of healthy women and can be transmitted to the baby during birth. Understanding the risks associated with GBS in pregnancy is crucial for expectant mothers to ensure the best possible outcomes for their babies.
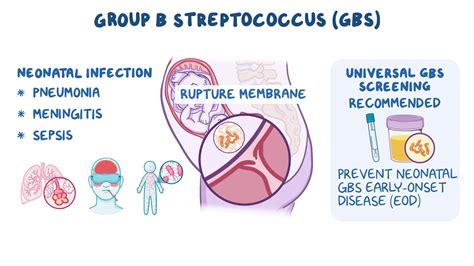
The importance of recognizing GBS in pregnancy cannot be overstated. While it may not cause symptoms in the mother, GBS can pose significant risks to the newborn, including serious infections such as sepsis, pneumonia, and meningitis. These conditions can lead to severe complications, including death, in newborns. Therefore, it is essential for pregnant women to be aware of their GBS status and take necessary precautions to minimize the risk of transmission to their babies.
GBS screening is a routine part of prenatal care, typically performed between 36 and 37 weeks of gestation. The test involves collecting a swab from the vagina and rectum to check for the presence of GBS. Women who test positive for GBS are considered colonized, meaning they carry the bacteria. This colonization does not necessarily mean the woman will pass the bacteria to her baby, but it does increase the risk. Understanding the results of the GBS test and the subsequent steps to be taken is vital for managing the risk effectively.
Understanding GBS Infection
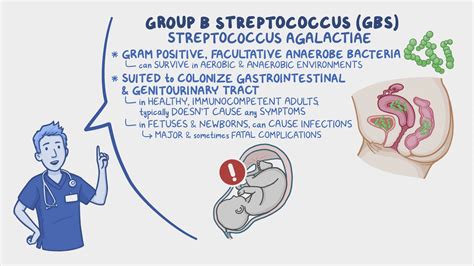
To comprehend the risks associated with GBS in pregnancy fully, it's essential to understand the nature of the infection itself. GBS is a common bacterium that can be found in up to 25% of healthy pregnant women. The bacteria are usually harmless to the mother but can be dangerous to the newborn if transmitted during delivery. The risk of transmission is higher in certain situations, such as if the mother has a fever during labor, if the water breaks more than 18 hours before delivery, or if the mother has a history of a previous baby with GBS disease.
Factors That Increase the Risk of GBS Transmission
Several factors can increase the risk of transmitting GBS to the baby during delivery. These include: - Preterm labor: Babies born before 37 weeks of gestation are at a higher risk. - Rupture of membranes: If the water breaks more than 18 hours before delivery, the risk increases. - Fever during labor: A temperature of 100.4°F (38°C) or higher can increase the risk. - Previous baby with GBS disease: If a previous baby has had GBS disease, the risk is higher for subsequent pregnancies. - GBS bacteriuria during pregnancy: If GBS is found in the urine during pregnancy, it indicates a heavier colonization and a higher risk.Prevention and Management of GBS in Pregnancy
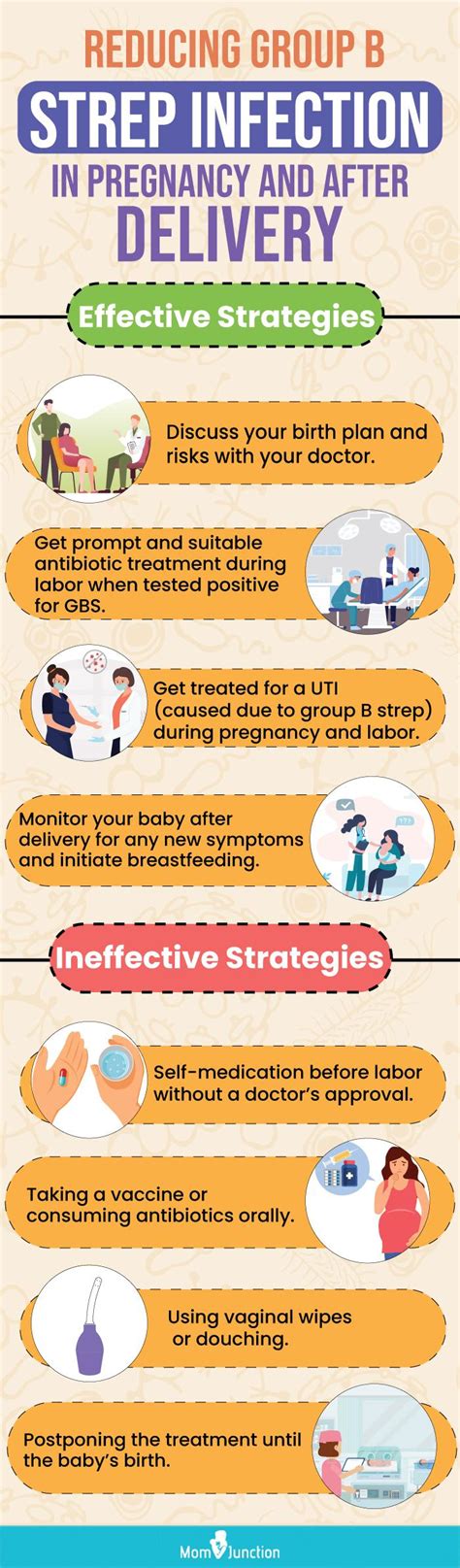
Preventing the transmission of GBS to the newborn is a critical aspect of prenatal care for women who test positive for the bacteria. The primary method of prevention is the administration of intravenous antibiotics during labor, which significantly reduces the risk of GBS transmission. It is essential for women to discuss their GBS status and any concerns with their healthcare provider to determine the best course of action.
For women who are GBS positive, the American College of Obstetricians and Gynecologists (ACOG) recommends intrapartum antibiotic prophylaxis (IAP) during labor. The antibiotics most commonly used are penicillin or ampicillin, given every 4 hours until delivery. This treatment is highly effective in reducing the risk of early-onset GBS disease in newborns.
Steps to Take If You're GBS Positive
If you test positive for GBS, here are some steps you can take: - Inform your healthcare provider: Ensure your healthcare provider knows your GBS status so they can plan your care accordingly. - Discuss antibiotic treatment: Talk to your healthcare provider about receiving antibiotics during labor to reduce the risk of transmission. - Understand the signs of GBS disease in newborns: Be aware of the signs of GBS disease in newborns, such as fever, lethargy, and difficulty feeding, and seek medical attention immediately if you notice any of these symptoms.GBS and Pregnancy Complications
While GBS itself may not cause pregnancy complications, the presence of the bacteria can increase the risk of certain conditions. For example, women with GBS bacteriuria during pregnancy are at a higher risk of preterm labor and low birth weight babies. Additionally, the risk of stillbirth may be increased in women with GBS colonization, although this is rare.
Understanding the potential complications associated with GBS in pregnancy is crucial for managing the risks effectively. Pregnant women should be vigilant about their health and report any concerns or symptoms to their healthcare provider promptly.
Pregnancy Complications Associated with GBS
Some pregnancy complications associated with GBS include: - Preterm labor: Women with GBS bacteriuria are at a higher risk of preterm labor. - Low birth weight: Babies born to mothers with GBS bacteriuria may have a lower birth weight. - Stillbirth: Although rare, the risk of stillbirth may be increased in women with GBS colonization.GBS Disease in Newborns
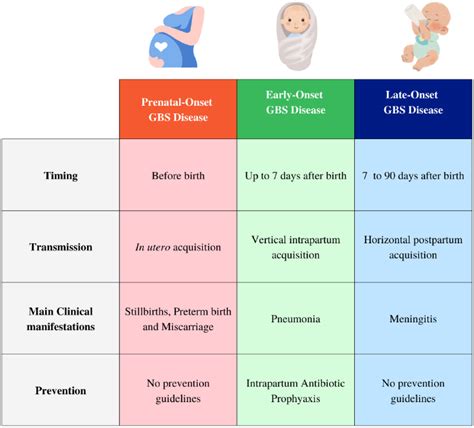
GBS disease in newborns can manifest in different forms, including sepsis, pneumonia, and meningitis. Early-onset GBS disease occurs within the first week of life, usually within the first 24 hours, and is typically associated with maternal transmission during delivery. Late-onset GBS disease occurs after the first week of life and is often associated with environmental exposure.
Recognizing the signs of GBS disease in newborns is critical for prompt medical intervention. Symptoms can include fever, lethargy, difficulty feeding, and respiratory distress. If you suspect your baby has GBS disease, seek medical attention immediately.
Symptoms of GBS Disease in Newborns
Symptoms of GBS disease in newborns may include: - Fever - Lethargy - Difficulty feeding - Respiratory distress - Apnea (pauses in breathing) - Bradycardia (slow heart rate)Conclusion and Next Steps

In conclusion, understanding the risks associated with GBS in pregnancy is vital for expectant mothers. By being aware of their GBS status and taking necessary precautions, women can significantly reduce the risk of transmitting the bacteria to their babies. It is essential to maintain open communication with healthcare providers and to be informed about the signs of GBS disease in newborns.
If you have any concerns or questions about GBS in pregnancy, do not hesitate to reach out to your healthcare provider. Share this article with friends and family who may benefit from this information, and consider joining support groups or online forums to connect with others who have experienced GBS in pregnancy.
What is Group B Streptococcus (GBS)?
+Group B Streptococcus (GBS) is a type of bacteria that can be found in the digestive and lower genital tracts of healthy women. It can be transmitted to the baby during birth and cause serious infections.
How is GBS diagnosed in pregnancy?
+GBS is diagnosed through a screening test performed between 36 and 37 weeks of gestation. The test involves collecting a swab from the vagina and rectum to check for the presence of GBS.
What are the symptoms of GBS disease in newborns?
+Symptoms of GBS disease in newborns may include fever, lethargy, difficulty feeding, respiratory distress, apnea, and bradycardia. If you suspect your baby has GBS disease, seek medical attention immediately.
