Intro
Discover 5 essential tips for a healthy GBS positive pregnancy, including prevention methods, symptoms management, and treatment options to minimize risks and ensure a safe delivery, Group B strep pregnancy complications, and prenatal care.
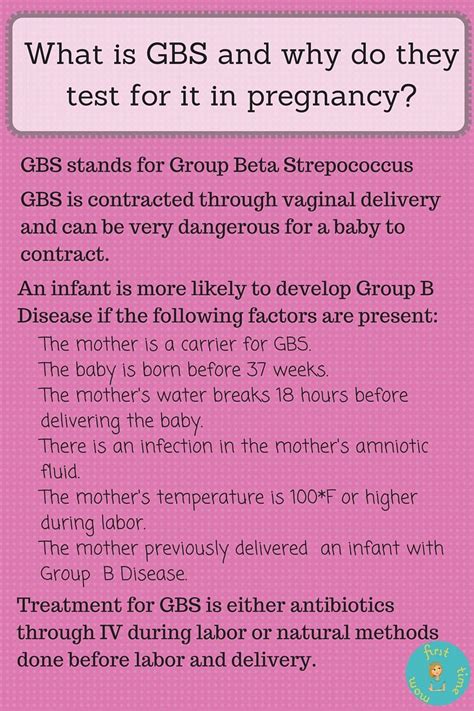
Pregnancy is a life-changing experience that brings immense joy and responsibility. For women who test positive for Group B Streptococcus (GBS), also known as GBS positive, it's essential to understand the implications and take necessary precautions to ensure a healthy pregnancy and childbirth. GBS is a common bacteria that can be present in the vagina and rectum of healthy women, but it can pose a risk to the baby during delivery. Here's an overview of what GBS positive pregnancy means and how to manage it.
GBS positive pregnancy requires careful monitoring and planning to minimize the risk of transmission to the baby. Women who test positive for GBS typically undergo routine testing between 35 and 37 weeks of gestation. If the test results are positive, the healthcare provider will discuss the best course of action to ensure a safe delivery. This may include administering antibiotics during labor to reduce the risk of transmission.
The importance of managing GBS positive pregnancy cannot be overstated. According to the Centers for Disease Control and Prevention (CDC), GBS is a leading cause of illness and death among newborns. However, with proper care and precautions, the risk of transmission can be significantly reduced. In this article, we will delve into the world of GBS positive pregnancy, exploring the causes, symptoms, diagnosis, treatment, and management strategies.
Understanding GBS Positive Pregnancy

Causes and Risk Factors
The exact causes of GBS positive pregnancy are not fully understood, but several risk factors have been identified. These include: * Previous GBS infection * History of GBS positive pregnancy * African American ethnicity * Age under 20 or over 35 * Multiple pregnancy (twins, triplets, etc.) * Preterm labor * Rupture of membranes more than 18 hours before deliveryDiagnosis and Testing

Types of Tests
There are two types of tests used to diagnose GBS positive pregnancy: * PCR (polymerase chain reaction) test: This test detects the genetic material of the GBS bacteria. * Culture test: This test involves growing the bacteria in a laboratory to confirm the presence of GBS.Management and Treatment
Antibiotic Prophylaxis
Antibiotic prophylaxis is the use of antibiotics to prevent the transmission of GBS to the baby during delivery. The antibiotics are typically administered intravenously during labor, and the most commonly used antibiotics are penicillin and ampicillin.5 Tips for GBS Positive Pregnancy
Additional Tips
Additional tips for managing GBS positive pregnancy include: * Practicing good hygiene to reduce the risk of transmission * Avoiding unnecessary interventions during labor * Considering a doula or birth support person to provide emotional support during laborConclusion and Next Steps

What is GBS positive pregnancy?
+GBS positive pregnancy occurs when a woman tests positive for Group B Streptococcus bacteria, which can pose a risk to the baby during delivery.
How is GBS positive pregnancy diagnosed?
+Diagnosing GBS positive pregnancy typically involves a routine test between 35 and 37 weeks of gestation, which involves collecting a sample from the vagina and rectum and sending it to a laboratory for analysis.
What are the risks of GBS positive pregnancy?
+The risks of GBS positive pregnancy include transmission of the bacteria to the baby during delivery, which can cause illness and death in newborns.
How is GBS positive pregnancy managed?
+Managing GBS positive pregnancy involves careful monitoring and planning to minimize the risk of transmission to the baby, which may include administering antibiotics during labor and considering a cesarean delivery.
What can I do to reduce the risk of transmission?
+To reduce the risk of transmission, follow your healthcare provider's advice, take antibiotics as prescribed, and practice good hygiene to reduce the risk of transmission.
We hope this article has provided you with valuable information and insights into GBS positive pregnancy. If you have any further questions or concerns, please don't hesitate to reach out to your healthcare provider or a prenatal care expert. Share your thoughts and experiences in the comments below, and don't forget to share this article with friends and family who may be interested in learning more about GBS positive pregnancy.
