Intro
Discover 5 key gestational diabetes causes, including hormonal changes, genetic predisposition, and obesity, to understand risk factors and manage blood sugar levels during pregnancy.
Gestational diabetes is a type of diabetes that develops during pregnancy, typically in the second or third trimester. It is a significant health concern for pregnant women, as it can increase the risk of complications for both the mother and the baby. Understanding the causes of gestational diabetes is essential for preventing and managing the condition. In this article, we will delve into the 5 main causes of gestational diabetes, exploring the risk factors, symptoms, and treatment options.
The importance of understanding gestational diabetes cannot be overstated. According to the American Diabetes Association, gestational diabetes affects up to 9.2% of pregnant women in the United States. If left untreated, gestational diabetes can lead to serious health complications, including high blood pressure, preeclampsia, and cesarean delivery. Moreover, babies born to mothers with gestational diabetes are at a higher risk of being overweight, having low blood sugar, and developing type 2 diabetes later in life.
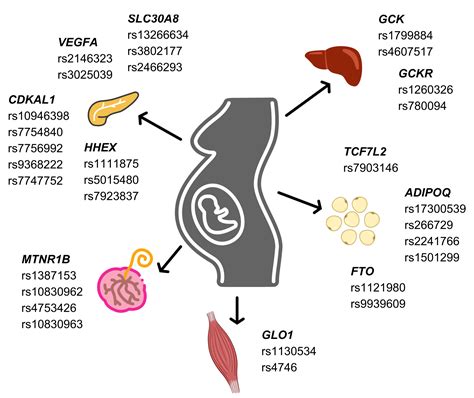
As we explore the causes of gestational diabetes, it is essential to recognize the interplay between genetic, hormonal, and lifestyle factors. While some risk factors are beyond our control, others can be mitigated through healthy lifestyle choices and medical interventions. By understanding the underlying causes of gestational diabetes, we can take proactive steps to prevent and manage the condition, ensuring a healthy pregnancy and a positive outcome for both mother and baby.
Gestational Diabetes and Hormonal Changes
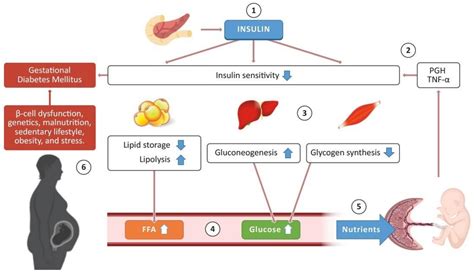
Insulin Resistance and Gestational Diabetes
Insulin resistance is a critical factor in the development of gestational diabetes. When the body becomes resistant to insulin, it produces more insulin to compensate, leading to high blood sugar levels. Insulin resistance can be caused by a combination of genetic and lifestyle factors, including obesity, physical inactivity, and a diet high in sugar and refined carbohydrates. Understanding the role of insulin resistance in gestational diabetes is essential for developing effective treatment and prevention strategies.Genetic Predisposition and Gestational Diabetes
Lifestyle Factors and Gestational Diabetes
Lifestyle factors, such as diet and physical activity, can significantly impact the risk of developing gestational diabetes. A diet high in sugar, refined carbohydrates, and saturated fats can contribute to insulin resistance and high blood sugar levels. Additionally, physical inactivity can exacerbate insulin resistance, making it more challenging to manage blood sugar levels. On the other hand, a healthy diet and regular physical activity can help mitigate the risk of gestational diabetes and improve overall health outcomes.Obesity and Gestational Diabetes

Age and Gestational Diabetes
Age is another significant risk factor for gestational diabetes. Women over the age of 35 are at a higher risk of developing gestational diabetes, particularly if they have other risk factors such as obesity or a family history of diabetes. Additionally, women who have had gestational diabetes in a previous pregnancy are more likely to develop it again in subsequent pregnancies. Understanding the role of age in gestational diabetes can help healthcare providers identify high-risk patients and develop targeted prevention and treatment strategies.Preventing Gestational Diabetes
Managing Gestational Diabetes
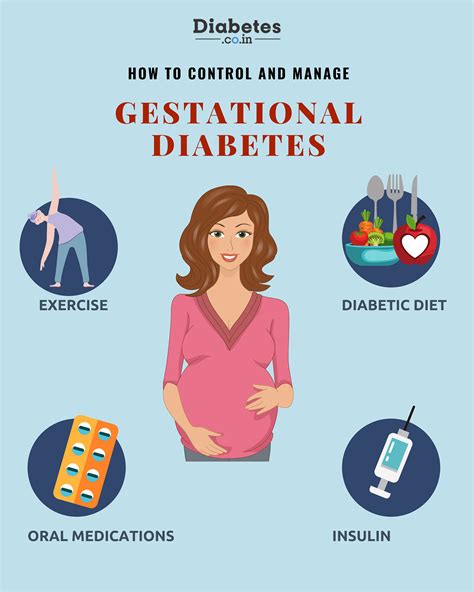
For women who develop gestational diabetes, managing the condition is critical for ensuring a healthy pregnancy and preventing long-term health complications. This typically involves working with a healthcare provider to develop a personalized treatment plan, which may include dietary changes, physical activity, and insulin therapy. Additionally, women with gestational diabetes should be closely monitored for any signs of complications, such as high blood pressure or preeclampsia, and should receive regular prenatal care to ensure the best possible outcomes for both mother and baby.Treatment Options for Gestational Diabetes
Long-Term Health Implications
Gestational diabetes can have long-term health implications for both mother and baby. Women who develop gestational diabetes are at a higher risk of developing type 2 diabetes later in life, as well as other health complications such as heart disease and stroke. Additionally, babies born to mothers with gestational diabetes are at a higher risk of being overweight, having low blood sugar, and developing type 2 diabetes later in life. Understanding the long-term health implications of gestational diabetes is essential for developing effective prevention and treatment strategies.What are the symptoms of gestational diabetes?
+The symptoms of gestational diabetes may include increased thirst and urination, fatigue, blurred vision, and recurring infections. However, many women with gestational diabetes do not experience any noticeable symptoms, making regular blood sugar monitoring essential for diagnosis and management.
How is gestational diabetes diagnosed?
+Gestational diabetes is typically diagnosed between 24 and 28 weeks of pregnancy using a glucose screening test. If the results are abnormal, a follow-up glucose tolerance test may be necessary to confirm the diagnosis.
Can gestational diabetes be prevented?
+While some risk factors for gestational diabetes are beyond our control, there are several steps that can be taken to prevent the condition. Maintaining a healthy weight, eating a balanced diet, and engaging in regular physical activity can help mitigate the risk of gestational diabetes.
What are the treatment options for gestational diabetes?
+The treatment options for gestational diabetes depend on the severity of the condition and the individual needs of the patient. Lifestyle interventions, insulin therapy, and close monitoring of blood sugar levels are common treatment strategies for managing gestational diabetes.
What are the long-term health implications of gestational diabetes?
+Gestational diabetes can have long-term health implications for both mother and baby. Women who develop gestational diabetes are at a higher risk of developing type 2 diabetes later in life, as well as other health complications such as heart disease and stroke. Additionally, babies born to mothers with gestational diabetes are at a higher risk of being overweight, having low blood sugar, and developing type 2 diabetes later in life.
In conclusion, gestational diabetes is a significant health concern for pregnant women, and understanding the causes and risk factors is essential for preventing and managing the condition. By recognizing the interplay between genetic, hormonal, and lifestyle factors, we can take proactive steps to mitigate the risk of gestational diabetes and ensure a healthy pregnancy and positive outcome for both mother and baby. If you have any questions or concerns about gestational diabetes, we encourage you to comment below or share this article with others who may be affected by this condition. Together, we can work towards creating a healthier and more informed community for pregnant women and their families.
