Intro
Learn how to use an incentive spirometer with our comprehensive guide, improving lung function and respiratory health through breathing exercises and therapy, enhancing pulmonary rehabilitation.
The use of incentive spirometers has become a crucial component in the field of respiratory care, particularly for patients who have undergone surgery, are suffering from respiratory conditions, or are in the process of recovering from illnesses that affect the lungs. These devices are designed to help patients improve the functioning of their lungs, increase oxygen levels in the blood, and prevent complications such as pneumonia or atelectasis. Understanding how to use an incentive spirometer effectively is essential for both healthcare professionals and patients to ensure the best possible outcomes.
The importance of proper lung function cannot be overstated, as it directly impacts a patient's overall health and well-being. Incentive spirometers provide a simple, yet effective way to encourage patients to take an active role in their respiratory care. By using these devices, patients can learn how to breathe more deeply and effectively, which can lead to a faster recovery, reduced risk of respiratory complications, and improved quality of life. Moreover, the educational aspect of incentive spirometers helps patients understand the significance of their lung function and how it relates to their overall health, fostering a sense of responsibility and engagement in their care.
For healthcare providers, incorporating incentive spirometers into treatment plans offers a valuable tool for monitoring patient progress, setting realistic goals, and adjusting therapies as needed. The data provided by these devices can help in assessing the effectiveness of current treatments and in making informed decisions regarding future care. Furthermore, the use of incentive spirometers aligns with patient-centered care principles, empowering patients to participate actively in their recovery process. This not only enhances patient satisfaction but also contributes to better health outcomes, as engaged patients are more likely to adhere to their treatment plans and make necessary lifestyle adjustments.
Incentive Spirometer Basics
Understanding the basics of an incentive spirometer is the first step in its effective use. An incentive spirometer is a handheld device that measures how much air a patient can breathe in and out. It typically consists of a tube that the patient breathes through, connected to a meter that displays the volume of air moved. Some models may also include additional features such as digital displays, goal-setting mechanisms, or alarms to encourage patients to meet their targets. The core principle behind these devices is to provide visual feedback to patients, showing them the volume of air they are moving, which serves as an incentive to improve their breathing efforts.
Key Components of Incentive Spirometers
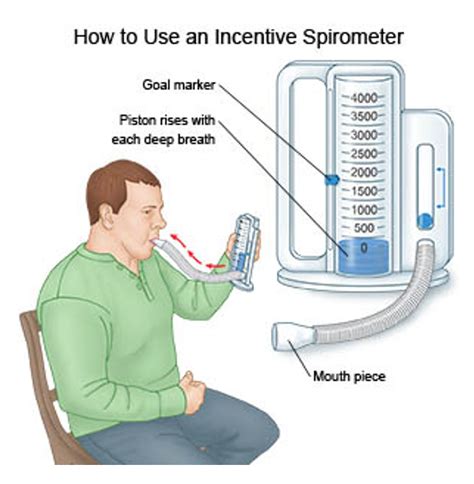
The key components of incentive spirometers include the breathing tube, the flow meter or volume display, and sometimes, a goal-setting feature. The breathing tube is where the patient inhales and exhales, and it is usually connected to a one-way valve to prevent air from escaping back into the device. The flow meter or volume display shows the patient how much air they have moved, providing immediate feedback on their performance. For models with goal-setting features, patients can set targets for themselves, and the device will indicate when these targets are met, offering a sense of accomplishment and motivation to continue improving.How to Use an Incentive Spirometer

Using an incentive spirometer involves several steps that patients should follow to maximize its benefits. First, the patient should sit upright in a comfortable position, with their back straight. This posture helps in achieving the most efficient breathing pattern. Next, the patient should hold the spirometer with both hands, placing the mouthpiece in their mouth, and closing their lips tightly around it to prevent air leakage. Then, they should inhale slowly and deeply through the mouthpiece, aiming to reach or surpass their target volume as indicated on the device. It's crucial to breathe slowly and steadily, as rapid breathing can lead to inaccurate readings and decreased effectiveness. After reaching the peak inhalation, the patient should hold their breath for a few seconds before exhaling slowly. This process should be repeated several times, with rests in between to avoid fatigue.
Tips for Effective Use
For effective use of an incentive spirometer, patients should practice regularly, ideally 5-10 times per session, several times a day. Consistency is key to seeing improvements in lung function. Patients should also aim to increase their inhalation volume gradually over time, setting realistic goals based on their progress. It's also important to note that patients should not push themselves too hard, as this can lead to discomfort or even injury. If any pain or difficulty is experienced, the patient should stop and consult with their healthcare provider.Benefits of Incentive Spirometry
The benefits of using incentive spirometry are multifaceted and significant. One of the primary advantages is the improvement in lung expansion and function. By encouraging patients to breathe more deeply and regularly, incentive spirometers help in preventing the collapse of lung tissue, a common issue in post-surgical patients or those with respiratory diseases. This can lead to a reduction in the risk of developing pneumonia or other respiratory complications, which are major concerns in these patient populations. Moreover, the use of incentive spirometers can result in shorter hospital stays, as patients who can breathe more effectively and efficiently tend to recover faster. The psychological benefits should also not be underestimated, as the sense of control and achievement that comes from meeting breathing goals can significantly boost a patient's morale and motivation during the recovery process.
Impact on Patient Recovery
The impact of incentive spirometry on patient recovery is profound. By facilitating better lung function, these devices contribute to improved oxygenation of the body's tissues, which is essential for healing and overall health. Patients who use incentive spirometers tend to have fewer respiratory complications, which in turn can lead to a reduction in the need for additional treatments or interventions, such as oxygen therapy or mechanical ventilation. Furthermore, the educational component of incentive spirometry empowers patients with the knowledge and skills necessary to manage their respiratory health effectively, promoting long-term wellness and reducing the risk of future complications.Common Applications of Incentive Spirometers

Incentive spirometers are used in a variety of clinical settings and patient populations. Post-surgical patients, especially those who have undergone abdominal or thoracic surgery, benefit significantly from the use of these devices. The deep breathing exercises encouraged by incentive spirometers help in preventing atelectasis, a condition where lung tissue collapses, and reducing the risk of pneumonia, both of which are common complications following surgery. Additionally, patients with chronic respiratory diseases such as chronic obstructive pulmonary disease (COPD) or asthma can use incentive spirometers as part of their management plan, helping them to improve lung function and control symptoms more effectively.
Use in Respiratory Rehabilitation
In the context of respiratory rehabilitation, incentive spirometers play a critical role. These programs are designed for patients with chronic respiratory conditions and aim to improve their quality of life through a combination of exercises, education, and support. Incentive spirometers are valuable tools in these programs, as they provide patients with a clear, measurable goal to work towards, which can be highly motivating. By incorporating incentive spirometry into rehabilitation plans, healthcare providers can help patients achieve significant improvements in their lung function, exercise tolerance, and overall health status, enabling them to lead more active and fulfilling lives.Choosing the Right Incentive Spirometer

Selecting the appropriate incentive spirometer for a patient's needs is crucial for its effective use. Healthcare providers should consider several factors, including the patient's specific respiratory condition, their current lung function, and any physical or cognitive limitations that might affect their ability to use the device. For example, patients with severe respiratory disease may require a spirometer that can measure very low volumes of air, while patients with arthritis might need a device with an easy-to-grip design. Additionally, the cost and availability of the device, as well as any insurance coverage, should be taken into account. It's also important to choose a spirometer that is easy to clean and maintain, to prevent the risk of infection.
Features to Consider
When evaluating different incentive spirometers, several features should be considered. The device should be easy to use and understand, with clear instructions and a simple interface. It should also be durable and able to withstand regular use. The accuracy of the device in measuring lung volumes is critical, and it should be calibrated regularly to ensure reliability. Some patients may prefer digital spirometers that offer additional features such as memory to track progress over time, alarms to remind them to practice, or the ability to set personalized goals. The availability of these features can vary between models, and healthcare providers should assess which features are most beneficial for their patients' specific needs.Maintenance and Cleaning of Incentive Spirometers

Proper maintenance and cleaning of incentive spirometers are essential to ensure their effectiveness and prevent the spread of infections. Patients should be instructed on how to clean their spirometer regularly, typically after each use. This can involve washing the mouthpiece and tube with soap and water, and then rinsing and drying them thoroughly. Some parts of the spirometer may be dishwasher safe, but this should be confirmed with the manufacturer's instructions. It's also important to disinfect the device periodically, using a disinfectant solution as recommended by the manufacturer. Regular maintenance, such as checking for blockages or damage, and calibrating the device as needed, is also crucial for ensuring the spirometer's accuracy and reliability.
Importance of Hygiene
The importance of maintaining good hygiene when using an incentive spirometer cannot be overstated. Respiratory devices can harbor bacteria and other pathogens, which can lead to infections if not properly cleaned and disinfected. Patients with compromised immune systems or those with chronic respiratory conditions are particularly vulnerable to these risks. By following a rigorous cleaning and maintenance routine, patients can significantly reduce the risk of infection and ensure that their incentive spirometer remains a safe and effective tool in their respiratory care.Training and Education

Training and education are vital components of effective incentive spirometer use. Patients should receive clear, comprehensive instructions on how to use their device, including how to assemble it, perform breathing exercises, and interpret the results. This education should be provided by a healthcare professional, such as a respiratory therapist or nurse, who can also address any questions or concerns the patient may have. Additionally, patients should be taught how to maintain and clean their spirometer, as well as how to troubleshoot any issues that may arise. Ongoing support and follow-up appointments can help ensure that patients are using their spirometer correctly and effectively, and can provide opportunities for adjusting the treatment plan as needed.
Role of Healthcare Providers
Healthcare providers play a critical role in the training and education of patients using incentive spirometers. They should assess the patient's understanding of the device and its use, and provide additional instruction or support as necessary. Regular follow-up appointments can help in monitoring the patient's progress, addressing any challenges they are facing, and making adjustments to the treatment plan to optimize outcomes. Furthermore, healthcare providers should be available to answer questions and provide guidance, fostering a collaborative relationship with the patient and promoting a sense of security and support throughout the recovery or management process.Future Developments in Incentive Spirometry

The field of incentive spirometry is continually evolving, with advancements in technology and our understanding of respiratory physiology leading to the development of new and innovative devices. Future developments are likely to include more sophisticated digital spirometers that can provide detailed analysis of a patient's breathing patterns, offer personalized coaching and feedback, and integrate with other healthcare technologies to enhance patient care. Additionally, there may be a greater focus on developing spirometers that are specifically tailored to the needs of different patient populations, such as pediatric or geriatric patients, who may have unique requirements and challenges.
Emerging Trends
Emerging trends in incentive spirometry include the incorporation of mobile and wireless technologies, allowing for real-time monitoring and feedback. This can enable healthcare providers to track a patient's progress remotely, making adjustments to the treatment plan as needed, and can also facilitate communication between patients and their healthcare team. Another trend is the development of gamification and virtual reality technologies that can make breathing exercises more engaging and enjoyable, potentially increasing patient adherence and motivation. These innovations have the potential to revolutionize the field of respiratory care, offering new and exciting opportunities for improving patient outcomes and enhancing the overall quality of care.What is an incentive spirometer and how does it work?
+An incentive spirometer is a device used to help patients improve the functioning of their lungs. It works by measuring how much air a patient can breathe in and out, providing visual feedback that serves as an incentive to improve breathing efforts.
Who can benefit from using an incentive spirometer?
+Patients who have undergone surgery, are recovering from respiratory illnesses, or have chronic respiratory conditions such as COPD or asthma can benefit from using an incentive spirometer. It helps in improving lung function, preventing complications, and enhancing overall recovery and management of respiratory health.
How often should I use an incentive spirometer?
+The frequency of using an incentive spirometer can vary depending on the patient's condition and the healthcare provider's recommendations. Generally, patients are advised to practice with the spirometer several times a day, with multiple repetitions per session, to see consistent improvement in lung function.
Can I use an incentive spirometer on my own, or do I need supervision?
+While patients can use an incentive spirometer on their own, initial supervision and instruction from a healthcare provider are recommended to ensure proper use and understanding of the device. Ongoing support and follow-up appointments can also be beneficial for monitoring progress and addressing any questions or concerns.
How do I clean and maintain my incentive spirometer?
+Cleaning and maintaining an incentive spirometer involves washing the mouthpiece and tube with soap and water, rinsing and drying them thoroughly, and periodically disinfecting the device. Regular checks for blockages or damage and calibration as needed are also important for ensuring the spirometer's accuracy and reliability.
As we conclude our exploration of incentive spirometry, it's clear that these devices offer a powerful tool in the management and recovery of respiratory health. By understanding how to use an incentive spirometer effectively, patients can take a proactive role in their care, working towards improved lung function, reduced risk of complications, and enhanced overall well-being. We invite readers to share their experiences with incentive spirometry, ask questions, or seek further information on this topic, contributing to a community of individuals dedicated to advancing respiratory care and improving patient outcomes. Whether you are a healthcare professional, a patient, or simply someone interested in learning more about incentive spirometry, we hope this comprehensive guide has provided valuable insights and inspiration for your journey in respiratory health.
