Intro
Boost your understanding of reticulocyte count increases with 5 key methods, exploring anemia, blood disorders, and bone marrow function, to improve health outcomes.
The reticulocyte count is a crucial parameter in the field of hematology, used to assess the production of red blood cells by the bone marrow. An increase in reticulocyte count can be an indicator of various conditions, ranging from physiological responses to pathological states. Understanding the reasons behind an elevated reticulocyte count is essential for healthcare professionals to make accurate diagnoses and provide appropriate treatments. In this article, we will delve into the significance of reticulocyte count, its normal range, and explore five ways in which it can increase, along with practical examples and statistical data to support the explanations.
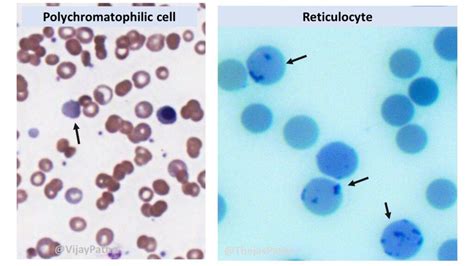
Reticulocytes are immature red blood cells that circulate in the blood for about a day before maturing into erythrocytes. The reticulocyte count, expressed as a percentage of total red blood cells, reflects the bone marrow's response to anemia or blood loss. Normally, the reticulocyte count ranges from 0.5% to 1.5% in adults, but this can vary depending on factors such as age, sex, and altitude. An elevated reticulocyte count suggests an increased production of red blood cells, which can be a response to various stimuli.
The importance of monitoring reticulocyte counts lies in its diagnostic and prognostic value. For instance, in cases of anemia, an elevated reticulocyte count can indicate that the bone marrow is actively producing red blood cells to compensate for the loss, which is a positive sign. Conversely, a low reticulocyte count in the presence of anemia may suggest a problem with red blood cell production, such as bone marrow failure. Thus, understanding the factors that influence reticulocyte count is crucial for managing patients with hematological disorders.
Introduction to Reticulocyte Count
Physiological Responses
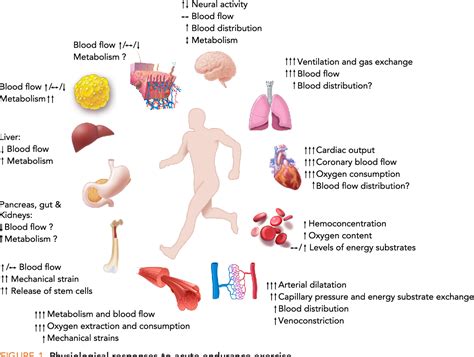
Adaptation to High Altitude
Adaptation to high altitude is a classic example of a physiological response leading to an increased reticulocyte count. At high elevations, the air pressure is lower, resulting in less oxygen being available to the body. To compensate, the kidneys produce more erythropoietin, which stimulates the bone marrow to produce more red blood cells. This increase in red blood cell production is reflected by an elevated reticulocyte count, which can be observed in individuals who travel to or live at high altitudes.Pregnancy and Increased Red Blood Cell Production
During pregnancy, the mother's body undergoes numerous changes to support the growing fetus. One of these changes is an increase in blood volume, which includes an increase in red blood cell mass. The reticulocyte count rises in response to the increased demand for oxygen and nutrients by the fetus. This physiological adaptation ensures that both the mother and the fetus receive adequate oxygenation and nutrients throughout the pregnancy.Pathological Conditions
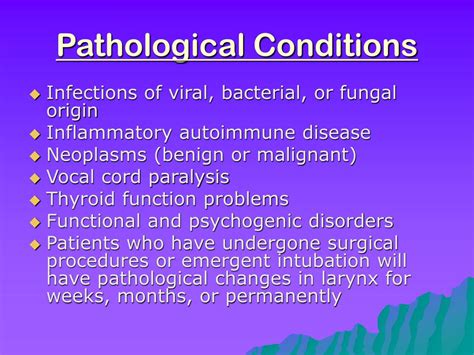
Anemia and Increased Reticulocyte Count
Anemia is characterized by a decrease in the number of red blood cells or the amount of hemoglobin in the blood. In response to anemia, the bone marrow increases the production of red blood cells, leading to an elevated reticulocyte count. The type of anemia can influence the reticulocyte count; for example, in iron deficiency anemia, the reticulocyte count may initially be low due to insufficient iron for erythropoiesis but increases with iron supplementation. In contrast, in hemolytic anemias, the reticulocyte count is typically elevated as the body tries to compensate for the ongoing destruction of red blood cells.Blood Loss and Hemolysis
Blood loss, whether acute or chronic, leads to a decrease in the number of circulating red blood cells. The body responds to this decrease by increasing the production of new red blood cells, reflected by an increase in reticulocyte count. Similarly, in conditions where red blood cells are being destroyed at an accelerated rate (hemolysis), such as in autoimmune hemolytic anemia or glucose-6-phosphate dehydrogenase (G6PD) deficiency, the reticulocyte count rises as the bone marrow attempts to keep pace with the destruction of red blood cells.Medications and Toxins
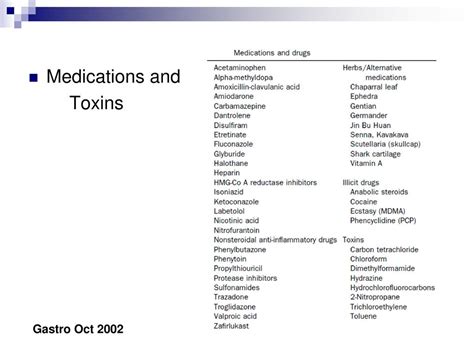
Erythropoietin-Stimulating Agents
Erythropoietin-stimulating agents (ESAs) are medications that mimic the action of erythropoietin, the natural hormone produced by the kidneys that stimulates red blood cell production. ESAs are used to treat anemia in patients with chronic kidney disease, cancer, and HIV infection. By stimulating the bone marrow to produce more red blood cells, ESAs can increase the reticulocyte count, which is a desired effect in the treatment of anemia but requires careful monitoring to avoid excessive erythrocytosis.Toxins and Drugs Causing Hemolysis
Certain drugs and toxins can cause hemolysis, either through an immune-mediated mechanism or by directly damaging the red blood cell membrane. Examples include certain antibiotics, anti-inflammatory drugs, and toxins like lead and arsenic. The body's response to hemolysis is to increase the production of red blood cells, which can result in an elevated reticulocyte count. Identifying and removing the causative agent is crucial in managing such conditions.Genetic Disorders
Hereditary Spherocytosis
Hereditary spherocytosis is a genetic disorder characterized by the production of red blood cells that are sphere-shaped rather than the normal biconcave disk shape. These abnormal red blood cells are prematurely destroyed in the spleen, leading to hemolytic anemia. The body's response to this ongoing hemolysis is to increase the production of new red blood cells, resulting in an elevated reticulocyte count. Treatment often involves splenectomy to reduce the destruction of red blood cells.Erythropoietin-Related Genetic Disorders
Genetic disorders affecting the erythropoietin gene or its receptor can influence the production of red blood cells. For example, mutations that lead to overproduction of erythropoietin can result in primary erythrocytosis, characterized by an excessive production of red blood cells. Conversely, mutations leading to underproduction or insensitivity to erythropoietin can result in anemia. The reticulocyte count can be affected in these conditions, either being elevated in response to increased erythropoietin levels or decreased in cases of erythropoietin deficiency.Conclusion and Future Directions

As we continue to explore the complexities of reticulocyte count and its implications for health and disease, it is essential to consider the broader context of hematological research. The interplay between genetic, environmental, and physiological factors influences red blood cell production and destruction, making the study of reticulocyte count a fascinating and multifaceted field. By engaging with the latest research and clinical findings, healthcare professionals and researchers can work together to advance our understanding of hematological disorders and develop innovative treatments.
What is the normal range for reticulocyte count?
+The normal range for reticulocyte count is typically between 0.5% and 1.5% of total red blood cells in adults, but this can vary slightly depending on the laboratory and the individual's specific conditions.
What does an elevated reticulocyte count indicate?
+An elevated reticulocyte count can indicate an increased production of red blood cells, which can be a response to anemia, blood loss, hemolysis, or other conditions where the body needs to replace red blood cells.
How is reticulocyte count measured?
+Reticulocyte count is measured through a blood test, where a sample of blood is drawn and analyzed for the presence of reticulocytes, typically expressed as a percentage of total red blood cells.
What are some common causes of an increased reticulocyte count?
+Common causes include recovery from anemia, blood loss, hemolysis, bone marrow stimulation, and certain medications or toxins that either stimulate red blood cell production or cause hemolysis.
Can genetic disorders affect reticulocyte count?
+Yes, genetic disorders such as hereditary spherocytosis or those affecting erythropoietin production can influence red blood cell production and, consequently, the reticulocyte count.
