Intro
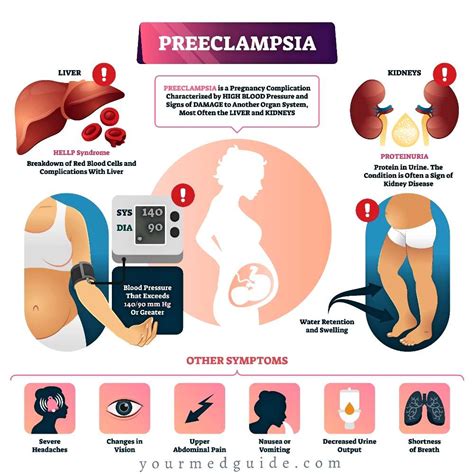
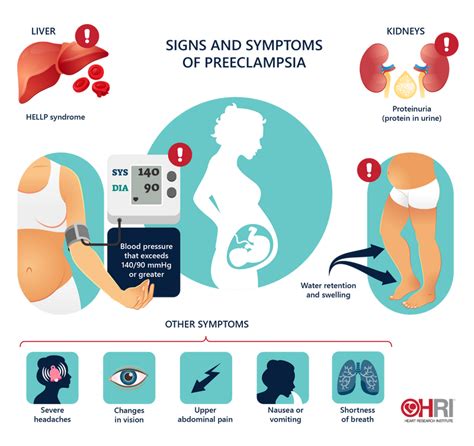
Identify 7 key preeclampsia symptoms, including high blood pressure, proteinuria, and severe headaches, to ensure timely diagnosis and treatment, preventing pregnancy complications like eclampsia and placental abruption.
Preeclampsia is a pregnancy complication characterized by high blood pressure and often accompanied by significant amounts of protein in the urine. This condition can lead to serious complications for both the mother and the baby if left untreated. It is crucial for pregnant women to be aware of the symptoms of preeclampsia to ensure early detection and proper management. The importance of recognizing these symptoms cannot be overstated, as timely medical intervention can significantly reduce the risk of severe complications.
The symptoms of preeclampsia can vary from one woman to another, and in some cases, the condition may develop without noticeable symptoms until it reaches an advanced stage. However, being informed about the common signs and seeking medical care promptly can make a significant difference in the outcome of the pregnancy. Preeclampsia affects a considerable number of pregnancies worldwide, making it a significant concern for maternal and fetal health. Understanding the risk factors and being vigilant about the symptoms are key steps in managing this condition effectively.
Preeclampsia can occur in any pregnancy, but certain factors increase the risk. These include a history of preeclampsia in a previous pregnancy, pre-existing hypertension, diabetes, kidney disease, and obesity. Women carrying twins or other multiples are also at a higher risk. Given the potential severity of preeclampsia, it is essential for all pregnant women to be aware of the symptoms and to attend prenatal appointments regularly, where their blood pressure and urine can be monitored.
Preeclampsia Overview
Causes and Risk Factors
The causes of preeclampsia are multifactorial and not entirely understood. However, several risk factors have been identified, including first pregnancy, carrying twins or other multiples, history of certain medical conditions like hypertension, diabetes, and kidney disease, and a history of preeclampsia in a previous pregnancy. Understanding these risk factors can help in identifying women who are at a higher risk and ensuring they receive closer monitoring during pregnancy.Symptoms of Preeclampsia
Diagnosing Preeclampsia
Diagnosing preeclampsia involves a combination of clinical evaluation, laboratory tests, and sometimes imaging studies. Regular prenatal check-ups are crucial for early detection, as they allow healthcare providers to monitor blood pressure and test urine for protein. If preeclampsia is suspected, further tests may be conducted to assess the severity of the condition and the well-being of the fetus. These tests can include blood tests to check for signs of kidney or liver damage, ultrasound scans to evaluate fetal growth and well-being, and non-stress tests to monitor fetal heart rate.Managing Preeclampsia
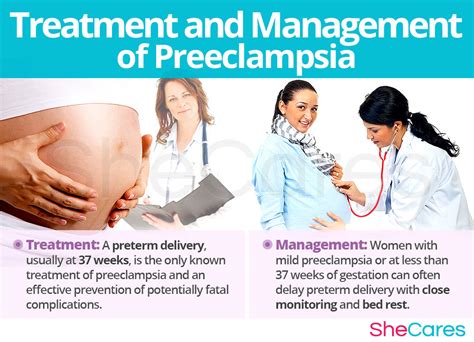
Treatment Options
Treatment for preeclampsia aims to prevent the condition from progressing and to ensure the best possible outcomes for both the mother and the baby. This may involve bed rest, although its effectiveness is debated, medications to lower blood pressure, corticosteroids to promote fetal lung maturity if preterm delivery is anticipated, and in severe cases, magnesium sulfate to prevent seizures. The decision on when to deliver the baby depends on the severity of the preeclampsia and the gestational age, balancing the risks of preterm birth against the risks of allowing the pregnancy to continue.Prevention Strategies

Lifestyle Modifications
Lifestyle modifications play a significant role in reducing the risk of preeclampsia and managing the condition if it develops. This includes dietary changes, such as increasing calcium intake, which some studies suggest may help reduce the risk of preeclampsia. Staying hydrated, avoiding excessive salt intake, and managing stress through techniques like meditation or deep breathing exercises can also be beneficial. For women at high risk, low-dose aspirin may be recommended under the guidance of a healthcare provider.Complications of Preeclampsia
Long-Term Implications
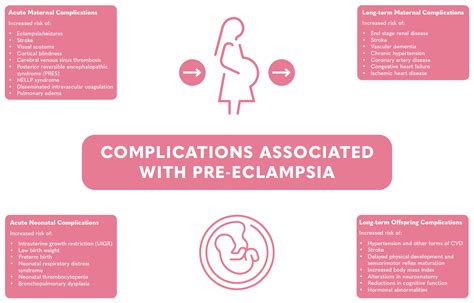
The long-term implications of preeclampsia can be significant for both mothers and babies. Women who have had preeclampsia are at a higher risk of developing cardiovascular disease and kidney disease later in life. Babies born to mothers with preeclampsia may have an increased risk of certain health issues, including high blood pressure, kidney disease, and learning disabilities. Therefore, follow-up care after pregnancy is crucial for monitoring and managing these potential long-term effects.Preeclampsia and Future Pregnancies
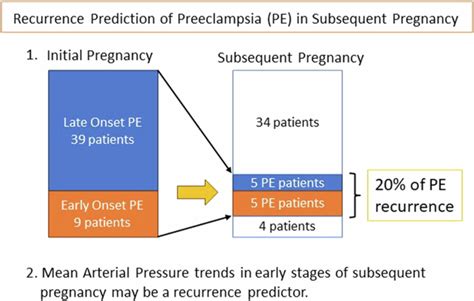
Planning for Future Pregnancies
Planning for future pregnancies after having preeclampsia involves several steps. This includes discussing the previous pregnancy history with a healthcare provider, understanding the risks and how they can be managed, and making lifestyle changes to reduce the risk of preeclampsia. Regular prenatal care is critical, and in some cases, low-dose aspirin may be recommended starting early in pregnancy to help prevent preeclampsia.Conclusion and Next Steps

We invite you to share your thoughts and experiences with preeclampsia in the comments below. If you found this article informative, please consider sharing it with others who may benefit from this information. Together, we can raise awareness about preeclampsia and promote healthier pregnancies.
What are the primary symptoms of preeclampsia?
+The primary symptoms of preeclampsia include high blood pressure, excess protein in the urine, severe headaches, vision changes, nausea and vomiting, and pain in the upper right abdomen.
How is preeclampsia diagnosed?
+Preeclampsia is diagnosed through a combination of clinical evaluation, laboratory tests such as urine protein checks, and sometimes imaging studies like ultrasound scans to assess fetal well-being.
Can preeclampsia be prevented?
+While there is no guaranteed way to prevent preeclampsia, maintaining a healthy lifestyle, including a balanced diet, regular physical activity, and managing stress, may help reduce the risk.
What are the potential long-term implications of preeclampsia for mothers and babies?
+Mothers who have had preeclampsia are at a higher risk of developing cardiovascular disease and kidney disease later in life. Babies may have an increased risk of high blood pressure, kidney disease, and learning disabilities.
How can women reduce their risk of developing preeclampsia in future pregnancies?
+Women can reduce their risk by maintaining a healthy weight, following a balanced diet, staying physically active, managing stress, and discussing their history and risk factors with their healthcare provider before becoming pregnant again.
