Intro
Discover 5 essential Strep B tips to prevent Group B strep infection, promoting maternal and newborn health with prenatal care, testing, and treatment options, ensuring a safe pregnancy and childbirth experience.
The importance of understanding Group B strep (GBS) cannot be overstated, especially for pregnant women and new parents. Group B strep is a common bacteria that can be found in the digestive and lower genital tracts of both men and women. While it is typically harmless in healthy adults, GBS can pose significant risks to newborns if they are exposed to it during birth. This is why being informed about GBS is crucial for expectant mothers and their healthcare providers. In this article, we will delve into the world of Group B strep, exploring its implications, prevention strategies, and management techniques.
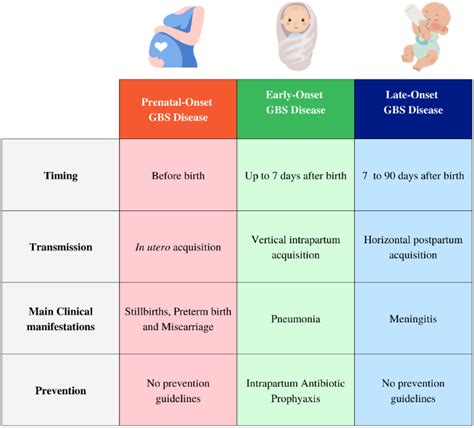
Understanding Group B strep is the first step towards mitigating its potential risks. It's essential to recognize that GBS is not a sexually transmitted infection, despite its presence in the genital tract. The bacteria can colonize in the body without causing any symptoms, making it challenging to detect without proper testing. Pregnant women who are colonized with GBS are at a higher risk of passing it to their babies during delivery. This transmission can lead to early-onset GBS infection in newborns, which may result in pneumonia, sepsis, or meningitis. The good news is that with proper prenatal care and management, the risk of GBS transmission can be significantly reduced.
The journey to managing Group B strep effectively begins with awareness and education. Expectant mothers should discuss their GBS status with their healthcare providers to understand their individual risks and develop a plan for a safe delivery. This plan may include antibiotic prophylaxis during labor, which has been shown to reduce the risk of early-onset GBS disease in newborns. Moreover, understanding the signs and symptoms of GBS infection in both mothers and babies is vital for prompt medical intervention. By empowering themselves with knowledge, pregnant women can play an active role in ensuring the best possible outcomes for their babies.
Introduction to Group B Strep
Risk Factors for GBS
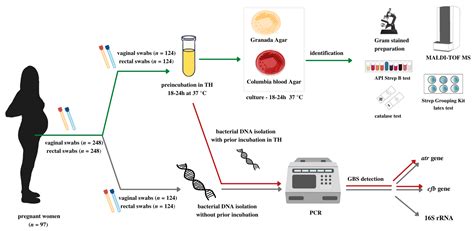
Several factors can increase the risk of a pregnant woman transmitting GBS to her baby. These include a previous history of GBS disease in a newborn, GBS bacteriuria during the current pregnancy, and a positive GBS screening result between 36 and 37 weeks of gestation. Additionally, women who have a fever during labor, those whose water breaks before 37 weeks of gestation, and those who have not received appropriate intrapartum antibiotic prophylaxis are at a higher risk. Recognizing these risk factors allows healthcare providers to offer targeted interventions to reduce the risk of GBS transmission.Screening and Testing for GBS
Understanding GBS Test Results
Interpreting GBS test results is straightforward: a positive result indicates the presence of GBS, while a negative result suggests that GBS is not present at the time of testing. However, it's crucial to remember that a negative test result does not guarantee that GBS will not be present at the time of delivery, as the colonization status can change. Therefore, even women with negative test results should be aware of the signs of GBS infection and seek medical attention immediately if they suspect any issues.Prevention and Management of GBS
Signs and Symptoms of GBS Infection
GBS infection in newborns can manifest as pneumonia, sepsis, or meningitis. The signs of GBS infection in babies may include refusal to feed, irritability, lethargy, fever, and difficulty breathing. In pregnant women, GBS infection can cause urinary tract infections, which may lead to preterm labor. Recognizing these signs and symptoms promptly can lead to timely medical intervention, reducing the risk of severe outcomes.Treatment Options for GBS
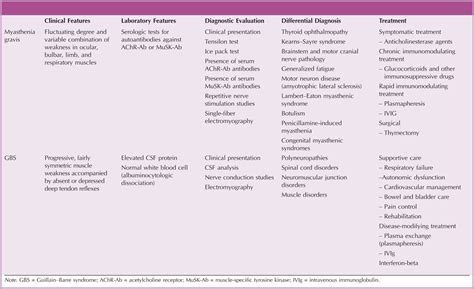
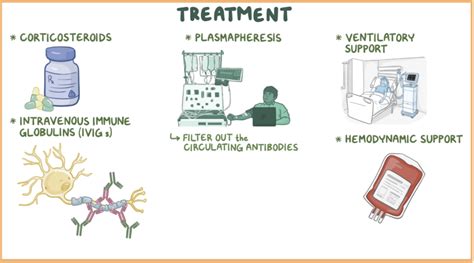
Supportive Care for GBS Infection
Supportive care plays a vital role in managing GBS infection, particularly in newborns. This care may include monitoring for signs of infection, maintaining proper hydration, and ensuring adequate oxygenation. In severe cases, babies may require admission to the neonatal intensive care unit (NICU) for close monitoring and treatment. The goal of supportive care is to help the body recover from the infection while minimizing potential complications.Living with GBS
Coping with GBS Diagnosis
Receiving a GBS diagnosis can be overwhelming, especially during pregnancy. However, it's essential to remember that with proper management, the risk of complications can be minimized. Women should focus on maintaining a healthy lifestyle, attending all scheduled prenatal appointments, and following the advice of their healthcare providers. Additionally, seeking support from family, friends, or support groups can help alleviate any anxiety or stress related to the diagnosis.Future Directions in GBS Management

Emerging Trends in GBS Research
Emerging trends in GBS research include the development of vaccines against Group B strep, which could potentially offer long-term protection against GBS colonization and infection. Additionally, there is a growing interest in the role of the microbiome in GBS colonization and the potential for probiotics or other microbiome-modulating therapies to prevent GBS. These areas of research hold promise for novel approaches to GBS management and prevention.What is Group B strep, and how common is it?
+Group B strep (GBS) is a common bacteria found in the digestive and lower genital tracts of both men and women. It is estimated that up to 30% of healthy pregnant women are colonized with GBS.
How is GBS transmitted to newborns?
+GBS is transmitted to newborns during delivery, as they pass through the birth canal. This can happen if the mother is colonized with GBS, especially if she has not received appropriate intrapartum antibiotic prophylaxis.
What are the symptoms of GBS infection in newborns?
+Symptoms of GBS infection in newborns can include refusal to feed, irritability, lethargy, fever, and difficulty breathing. If you suspect your baby has any of these symptoms, seek medical attention immediately.
How can GBS infection be prevented?
+GBS infection can be prevented through intrapartum antibiotic prophylaxis (IAP) for women who test positive for GBS. Maintaining good hygiene practices and recognizing the signs of GBS infection are also crucial for early intervention.
What is the treatment for GBS infection in newborns?
+The treatment for GBS infection in newborns typically involves antibiotics, which are administered intravenously. Supportive care, such as oxygen therapy and fluid management, may also be necessary.
As we conclude our exploration of Group B strep, it's clear that awareness, education, and proactive management are key to mitigating its risks. By understanding the implications of GBS, recognizing its signs and symptoms, and following recommended prevention and treatment strategies, pregnant women and their healthcare providers can work together to ensure the best possible outcomes for mothers and babies. We invite you to share your thoughts, experiences, or questions about Group B strep in the comments below, and to consider sharing this article with others who may benefit from this information. Together, we can promote a better understanding of GBS and support healthier pregnancies and newborns.
