Intro
Discover 5 ways RF test detects arthritis, leveraging radiofrequency to diagnose rheumatoid arthritis, osteoarthritis, and inflammatory joint diseases, using RF energy to assess joint health and inflammation.
Rheumatoid factor (RF) is an antibody that can be found in the blood of individuals with rheumatoid arthritis (RA), a chronic autoimmune disorder that primarily affects the joints. While not everyone with RA will test positive for RF, and not everyone with a positive RF test will have RA, the test remains a valuable tool in diagnosing and managing the condition. Understanding how RF tests for arthritis work, their limitations, and the broader context of diagnosing RA is crucial for both healthcare providers and patients.
The presence of RF can indicate an increased risk of developing RA or suggest that the condition is already present. However, RF can also be positive in individuals with other autoimmune diseases, infections, or even in healthy people, particularly as they age. This makes the interpretation of RF test results complex and necessitates a comprehensive approach to diagnosis that includes clinical evaluation, medical history, and potentially other diagnostic tests.
Rheumatoid arthritis is characterized by inflammation and pain in the joints, which can lead to severe disability if not properly managed. The symptoms of RA can vary significantly among individuals but often include morning stiffness, swelling, and warmth around the joints, and a general feeling of being unwell. The disease can also affect other body systems, such as the skin, eyes, lungs, heart, and blood vessels.
Understanding RF Tests
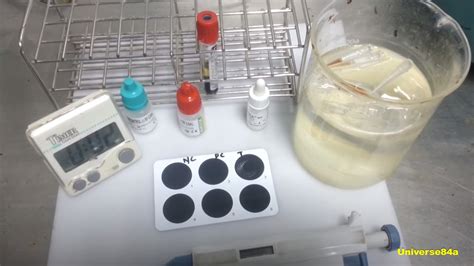
RF tests are blood tests used to detect the presence of rheumatoid factor in the blood. These tests can help diagnose rheumatoid arthritis but are not definitive on their own due to their lack of specificity. There are different types of RF tests, including those that measure IgM, IgG, and IgA rheumatoid factors. The most common type of RF is IgM RF, but detecting IgG and IgA RF can provide additional diagnostic information.
How RF Tests Work
RF tests work by identifying the presence of rheumatoid factor antibodies in the blood. These antibodies are directed against the Fc portion of IgG antibodies and can be of any immunoglobulin isotype (IgM, IgG, IgA). The tests typically involve mixing the patient's serum with IgG coated particles or wells. If RF is present, it binds to the IgG, and this binding can be detected using various laboratory techniques, such as nephelometry or enzyme-linked immunosorbent assay (ELISA).
Interpreting RF Test Results
Interpreting RF test results requires careful consideration of the clinical context. A positive RF test can indicate rheumatoid arthritis but also other conditions such as systemic lupus erythematosus (SLE), Sjögren's syndrome, and chronic infections. A negative RF test does not rule out RA, as up to 30% of patients with RA may be RF-negative. The titer (level) of RF can also provide information, with higher titers more commonly associated with RA.
Limitations of RF Tests
The limitations of RF tests include their low specificity for RA. Many conditions and even healthy individuals can have a positive RF test. Additionally, RF tests may not be positive early in the course of RA, leading to false-negative results in some patients. This underscores the importance of using RF tests as part of a broader diagnostic approach that includes clinical assessment, other laboratory tests (such as anti-citrullinated protein antibody [anti-CCP] tests), and imaging studies.
Diagnosing Rheumatoid Arthritis
Diagnosing rheumatoid arthritis involves a combination of clinical evaluation, laboratory tests, and imaging studies. The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) have developed classification criteria that include symptoms, serological tests (like RF and anti-CCP), and duration of symptoms. Early diagnosis is crucial for initiating appropriate treatment to prevent long-term damage and improve outcomes.
Steps in Diagnosing RA
- Clinical Assessment: Evaluating symptoms and signs, such as joint pain, swelling, and morning stiffness.
- Laboratory Tests: Including RF, anti-CCP, complete blood count (CBC), and erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) to assess inflammation.
- Imaging Studies: X-rays, ultrasound, and magnetic resonance imaging (MRI) to evaluate joint damage and inflammation.
Treatment and Management of RA

The treatment and management of RA aim to reduce inflammation, relieve symptoms, and prevent long-term damage. This typically involves a combination of medications, including disease-modifying antirheumatic drugs (DMARDs), biologic agents, and corticosteroids. Lifestyle modifications, such as maintaining a healthy diet, exercising regularly, and managing stress, are also important components of RA management.
Lifestyle Modifications for RA
- Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains.
- Exercise: Engaging in regular physical activity to maintain joint mobility and strength.
- Stress Management: Practicing stress-reducing techniques, such as meditation or yoga.
Future Directions in RF Testing and RA Management
Future directions in RF testing and RA management include the development of more specific and sensitive diagnostic tests, personalized treatment approaches based on genetic and environmental factors, and the exploration of new therapeutic targets. Advances in technology, such as the use of artificial intelligence and machine learning, may also improve the diagnosis and management of RA.
Emerging Trends in RA Research
- Precision Medicine: Tailoring treatment to the individual based on genetic, environmental, and lifestyle factors.
- Biomarkers: Identifying new biomarkers for early diagnosis and monitoring of RA.
- Immunotherapy: Exploring new immunotherapeutic approaches to modulate the immune system and reduce inflammation.
What is the primary use of RF tests in clinical practice?
+RF tests are primarily used to aid in the diagnosis of rheumatoid arthritis (RA) and to assess the risk of developing RA in individuals with undifferentiated arthritis.
Can RF tests be used to monitor the progression of RA?
+While RF tests can provide information on the presence of rheumatoid factor, they are not typically used to monitor the progression of RA. Other markers of inflammation, such as ESR and CRP, and clinical assessments are more commonly used for this purpose.
Are RF tests specific for rheumatoid arthritis?
+No, RF tests are not specific for rheumatoid arthritis. A positive RF test can be found in individuals with other autoimmune diseases, chronic infections, and even in healthy people, particularly as they age.
In conclusion, RF tests play a significant role in the diagnosis and management of rheumatoid arthritis, but their interpretation requires careful consideration of the clinical context and the use of a comprehensive diagnostic approach. As research continues to advance our understanding of RA and the role of RF, we can expect improvements in diagnostic accuracy and treatment outcomes. We invite readers to share their thoughts and experiences with RF testing and RA management, and to explore the resources available for further learning and support.
