Intro
Discover the 5 ways family physicians get paid, including fee-for-service, capitation, and value-based care, to understand physician compensation models and healthcare reimbursement methods.
Family physicians play a crucial role in the healthcare system, providing primary care to patients and coordinating their medical treatment. As with any profession, family physicians need to be compensated for their services. The payment methods for family physicians can vary depending on the healthcare system, location, and type of practice. Understanding how family physicians get paid is essential for patients, healthcare administrators, and policymakers. In this article, we will explore the different ways family physicians receive payment for their services.
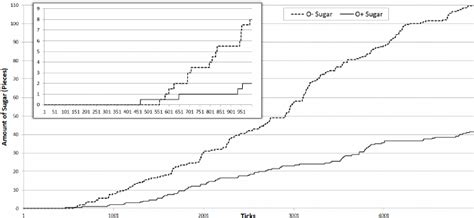
The way family physicians are paid can impact the quality of care they provide, their job satisfaction, and the overall efficiency of the healthcare system. Traditionally, family physicians have been paid on a fee-for-service basis, where they receive a payment for each consultation, procedure, or test they perform. However, this payment model has been criticized for incentivizing overutilization of services and neglecting preventive care. In recent years, there has been a shift towards alternative payment models that prioritize value-based care and population health.
The payment methods for family physicians can be complex and influenced by various factors, including government policies, insurance reimbursement rates, and practice settings. Family physicians may work in private practices, community health centers, hospitals, or academic institutions, each with its own payment structure. Moreover, the payment models may vary depending on the patient's insurance coverage, with Medicare, Medicaid, and private insurance companies having different reimbursement rates and requirements.
Fee-for-Service Payment Model

However, critics argue that this model can lead to overutilization of services, as physicians may order more tests or procedures to increase their revenue. Additionally, the fee-for-service model can neglect preventive care and chronic disease management, as these services may not be as lucrative as procedural services. Despite these limitations, the fee-for-service model remains the dominant payment method for family physicians, and it is often used in combination with other payment models.
Capitation Payment Model
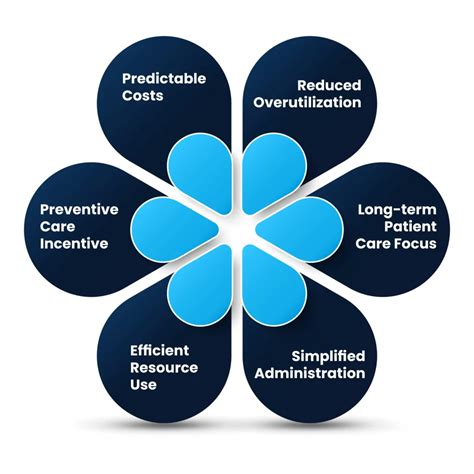
The capitation model provides an incentive for family physicians to provide preventive care and manage chronic diseases effectively, as they are responsible for the patient's overall health. However, this model can also create a risk for physicians, as they may be responsible for costly services or hospitalizations. To mitigate this risk, physicians may need to negotiate with specialists or hospitals to provide services at a discounted rate.
Value-Based Payment Model
The value-based payment model aims to improve the quality of care and reduce healthcare costs by promoting preventive care, chronic disease management, and coordination of care. This model requires family physicians to track and report their performance on quality metrics, which can be time-consuming and resource-intensive. However, the value-based payment model has the potential to improve patient outcomes and reduce healthcare disparities.
Pay-for-Performance Payment Model

The pay-for-performance model provides an incentive for family physicians to improve the quality of care and prioritize preventive services. However, this model can also create a risk for physicians, as they may be penalized for not meeting performance targets. To mitigate this risk, physicians may need to invest in quality improvement initiatives, such as electronic health records, patient registries, and care coordination programs.
Bundle Payment Model

The bundle payment model can be used for a variety of services, including chronic disease management, surgical procedures, and hospitalizations. This model requires family physicians to work closely with specialists, hospitals, and other healthcare providers to coordinate care and reduce costs. The bundle payment model has the potential to improve patient outcomes and reduce healthcare disparities, but it requires significant investment in care coordination and quality improvement initiatives.
In addition to these payment models, family physicians may also receive payment from other sources, such as patient copayments, coinsurance, and deductibles. The payment models may vary depending on the patient's insurance coverage, with Medicare, Medicaid, and private insurance companies having different reimbursement rates and requirements.
To illustrate the different payment models, consider the following examples:
- A family physician provides an office visit to a patient with diabetes, and the visit is reimbursed by Medicare at a rate of $100.
- A family physician provides a bundle of services related to diabetes care, including office visits, laboratory tests, and medications, and the bundle is reimbursed by a private insurance company at a rate of $500.
- A family physician meets quality targets for blood pressure control and patient satisfaction, and receives a bonus payment of $10,000 from a pay-for-performance program.
These examples illustrate the complexity of the payment models and the need for family physicians to navigate multiple reimbursement systems. However, by understanding the different payment models and their incentives, family physicians can provide high-quality care and improve patient outcomes while also managing their practice's finances effectively.
In terms of the benefits and drawbacks of each payment model, consider the following points:
- Fee-for-service model: benefits include simplicity and ease of use, but drawbacks include incentivizing overutilization of services and neglecting preventive care.
- Capitation model: benefits include promoting preventive care and chronic disease management, but drawbacks include creating a risk for physicians and requiring significant investment in care coordination.
- Value-based payment model: benefits include improving quality and reducing costs, but drawbacks include requiring significant investment in quality improvement initiatives and tracking performance metrics.
- Pay-for-performance model: benefits include incentivizing quality improvement, but drawbacks include creating a risk for physicians and requiring significant investment in quality improvement initiatives.
- Bundle payment model: benefits include promoting coordination of care and reducing costs, but drawbacks include requiring significant investment in care coordination and quality improvement initiatives.
Overall, the payment models for family physicians are complex and multifaceted, and they require significant investment in care coordination, quality improvement initiatives, and practice management. However, by understanding the different payment models and their incentives, family physicians can provide high-quality care and improve patient outcomes while also managing their practice's finances effectively.
Key Takeaways
The key takeaways from this article are: * Family physicians are paid using a variety of payment models, including fee-for-service, capitation, value-based, pay-for-performance, and bundle payment models. * Each payment model has its benefits and drawbacks, and they require significant investment in care coordination, quality improvement initiatives, and practice management. * The payment models can impact the quality of care and patient outcomes, and they require family physicians to navigate multiple reimbursement systems. * By understanding the different payment models and their incentives, family physicians can provide high-quality care and improve patient outcomes while also managing their practice's finances effectively.Conclusion and Next Steps
In conclusion, the payment models for family physicians are complex and multifaceted, and they require significant investment in care coordination, quality improvement initiatives, and practice management. However, by understanding the different payment models and their incentives, family physicians can provide high-quality care and improve patient outcomes while also managing their practice's finances effectively. The next steps for family physicians include: * Staying up-to-date with the latest developments in payment models and reimbursement systems. * Investing in care coordination and quality improvement initiatives to improve patient outcomes and reduce healthcare costs. * Navigating multiple reimbursement systems and managing practice finances effectively. * Providing high-quality care and improving patient outcomes while also managing practice finances effectively.What are the different payment models for family physicians?
+The different payment models for family physicians include fee-for-service, capitation, value-based, pay-for-performance, and bundle payment models.
How do payment models impact the quality of care and patient outcomes?
+Payment models can impact the quality of care and patient outcomes by incentivizing or disincentivizing certain behaviors, such as providing preventive care or ordering unnecessary tests.
What are the benefits and drawbacks of each payment model?
+The benefits and drawbacks of each payment model vary, but generally include benefits such as promoting preventive care and chronic disease management, and drawbacks such as creating a risk for physicians and requiring significant investment in care coordination and quality improvement initiatives.
