Intro
Discover Stevens Johnson Syndrome, a rare skin rash condition, characterized by severe allergic reactions, toxic epidermal necrolysis, and life-threatening symptoms, requiring prompt medical attention and treatment.
Stevens-Johnson Syndrome (SJS) is a rare but serious disorder of the skin and mucous membranes, usually caused by an adverse reaction to medications or infections. It is characterized by a skin rash, blisters, and peeling of the skin, which can be extremely painful and potentially life-threatening. SJS is often considered a medical emergency, requiring immediate attention and treatment. The importance of understanding SJS cannot be overstated, as prompt recognition and intervention can significantly improve outcomes and reduce the risk of long-term complications.
The skin rash associated with SJS is a critical aspect of the condition, as it can provide valuable clues for diagnosis and treatment. The rash typically begins as a red, flat patch on the skin, which can quickly progress to blisters, peeling, and open sores. In severe cases, the skin can become detached from the underlying tissue, leading to significant scarring and disfigurement. The rash can appear anywhere on the body, but it often affects the face, trunk, and extremities. It is essential to recognize the signs and symptoms of SJS, as early detection and treatment can make a significant difference in the outcome.
SJS is a complex condition, and its causes are not yet fully understood. However, research suggests that certain medications, such as antibiotics and anticonvulsants, can trigger an immune response that leads to the development of SJS. Infections, such as pneumonia and sepsis, can also contribute to the onset of the condition. Additionally, genetic factors may play a role in the development of SJS, as some individuals may be more susceptible to the condition due to their genetic makeup. Understanding the causes and risk factors associated with SJS is crucial for developing effective prevention and treatment strategies.
What is Stevens-Johnson Syndrome?

Symptoms of Stevens-Johnson Syndrome
The symptoms of SJS can vary in severity and may include: * A red, flat patch on the skin that quickly progresses to blisters, peeling, and open sores * Painful skin lesions that can appear anywhere on the body * Detachment of the skin from the underlying tissue, leading to significant scarring and disfigurement * Inflammation of the eyes, mouth, and genital areas * Fever, chills, and flu-like symptoms * Swollen lymph nodes and jointsCauses and Risk Factors of Stevens-Johnson Syndrome

Medications that Can Trigger Stevens-Johnson Syndrome
The following medications have been associated with an increased risk of SJS: * Antibiotics, such as penicillin and sulfonamides * Anticonvulsants, such as carbamazepine and phenytoin * Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen * Allopurinol, a medication used to treat goutDiagnosis and Treatment of Stevens-Johnson Syndrome
Wound Care for Stevens-Johnson Syndrome
Wound care is a critical aspect of treating SJS, as it can help promote healing, reduce the risk of infection, and minimize scarring. The following wound care strategies can be effective: * Debridement, or the removal of dead tissue and bacteria from the wound * Topical antibiotics and antiseptics to prevent infection * Moisturizers and dressings to promote healing and reduce scarring * Pain management, such as topical anesthetics and oral pain medicationsComplications and Prognosis of Stevens-Johnson Syndrome
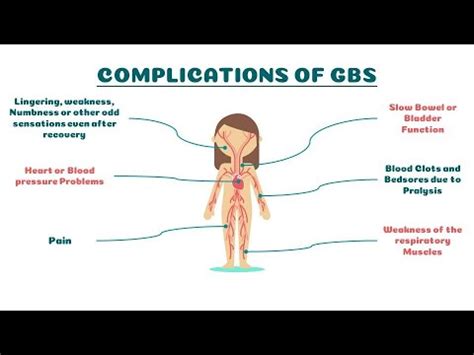
Long-Term Effects of Stevens-Johnson Syndrome
The long-term effects of SJS can be significant, including: * Scarring and disfigurement * Chronic pain and discomfort * Emotional and psychological trauma * Increased risk of infections and other complicationsPrevention and Management of Stevens-Johnson Syndrome

Support and Resources for Stevens-Johnson Syndrome
The following resources can provide support and guidance for individuals affected by SJS: * National Institutes of Health (NIH) * American Academy of Dermatology (AAD) * Stevens-Johnson Syndrome Foundation (SJSF) * Support groups and online forumsWhat are the symptoms of Stevens-Johnson Syndrome?
+The symptoms of SJS include a red, flat patch on the skin that quickly progresses to blisters, peeling, and open sores, painful skin lesions, detachment of the skin from the underlying tissue, inflammation of the eyes, mouth, and genital areas, fever, chills, and flu-like symptoms, and swollen lymph nodes and joints.
What causes Stevens-Johnson Syndrome?
+SJS is caused by an adverse reaction to medications or infections, which can trigger an immune response that leads to the development of the condition. Certain medications, such as antibiotics and anticonvulsants, can increase the risk of SJS, as can infections, such as pneumonia and sepsis.
How is Stevens-Johnson Syndrome treated?
+Treatment for SJS typically involves a multidisciplinary approach, including wound care, pain management, and supportive care. Wound care strategies, such as debridement, topical antibiotics, and moisturizers, can help promote healing and reduce the risk of infection. Pain management, such as topical anesthetics and oral pain medications, can help alleviate discomfort and promote comfort.
In conclusion, Stevens-Johnson Syndrome is a rare but potentially life-threatening condition that requires prompt recognition and treatment. Understanding the causes, symptoms, and treatment options for SJS is essential for improving outcomes and reducing the risk of long-term complications. By seeking medical attention promptly and following a comprehensive treatment plan, individuals affected by SJS can make a full recovery and minimize the risk of long-term effects. We invite you to share your experiences and ask questions about SJS in the comments below, and to explore the resources and support groups available for individuals affected by this condition.
