Intro
Discover 5 crucial Strep B facts, including symptoms, prevention, and treatment, to understand Group B strep infection, its risks, and pregnancy implications, and learn how to protect yourself and your baby from this common bacterial infection.
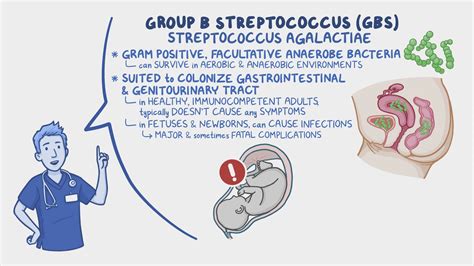
Group B streptococcus, commonly referred to as Group B strep or GBS, is a type of bacterial infection that can affect individuals of all ages, but it is most notably a concern for pregnant women and their newborns. The importance of understanding Group B strep lies in its potential to cause severe illness in newborns, highlighting the need for awareness and preventive measures. As we delve into the world of Group B strep, it becomes clear that knowledge is power, especially for expectant mothers who want to ensure the best possible health outcomes for their babies. The implications of GBS infection can be far-reaching, from mild to severe, making it crucial to grasp the basics and beyond of this bacterial infection.
The prevalence of Group B strep among pregnant women underscores the necessity for routine screening during pregnancy. This screening is a critical component of prenatal care, as it helps identify those at risk of passing the bacteria to their newborns during delivery. Understanding the risks and how they can be mitigated is essential for managing the health of both mother and baby. Moreover, the interplay between Group B strep and other health conditions can further complicate the situation, necessitating a comprehensive approach to healthcare during pregnancy. By exploring the intricacies of GBS, individuals can better navigate the complexities of prenatal care and make informed decisions about their health.
The journey to understanding Group B strep begins with acknowledging its presence and impact on public health. GBS is recognized as a leading cause of illness and death among newborns, making it a significant public health concern. However, with the right information and medical interventions, the risks associated with Group B strep can be significantly reduced. This balance between risk and prevention underscores the importance of education and awareness, not just for pregnant women but for the broader community. As we explore the facets of Group B strep, it becomes evident that a multifaceted approach, involving healthcare providers, expectant mothers, and the community, is essential for combating this bacterial infection.
What is Group B Strep?
Types of Group B Strep Infections
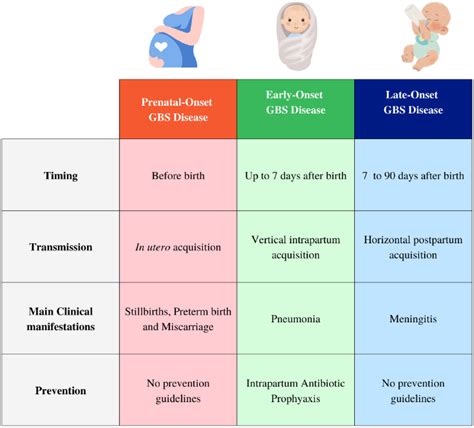
Group B strep infections can manifest in various ways, including urinary tract infections, bloodstream infections, and pneumonia. In pregnant women, GBS can cause infections of the uterus and amniotic fluid. Newborns, on the other hand, are at risk of developing early-onset GBS, which occurs within the first week of life, and late-onset GBS, which occurs after the first week. The severity and outcomes of these infections can vary widely, emphasizing the need for prompt medical attention if symptoms arise.Group B Strep Screening and Diagnosis
Importance of Prenatal Care
Prenatal care plays a vital role in the management of Group B strep. Regular check-ups allow healthcare providers to monitor the pregnancy, perform necessary screenings, and provide guidance on maintaining a healthy pregnancy. For women who are at high risk of GBS or have tested positive, prenatal care offers an opportunity for close monitoring and the implementation of preventive measures. This proactive approach can significantly reduce the risks associated with Group B strep, ensuring a healthier outcome for both mother and baby.Prevention and Treatment of Group B Strep

Role of Antibiotics in Prevention
Antibiotics play a crucial role in the prevention of Group B strep transmission. Penicillin and ampicillin are commonly used for this purpose, administered intravenously during labor. The timing and dosage of these antibiotics are critical, as they must be given at least four hours before delivery to be most effective. For women with a penicillin allergy, alternative antibiotics such as clindamycin or vancomycin may be used. The decision to use antibiotics should be made in consultation with a healthcare provider, considering the individual's medical history and the presence of any allergies.Living with Group B Strep
Coping with the Diagnosis
Receiving a diagnosis of Group B strep can be overwhelming, especially for expectant mothers. It is important to remember that with proper management and preventive care, the risks associated with GBS can be minimized. Staying informed, following healthcare provider recommendations, and maintaining open communication with medical professionals can help alleviate concerns and ensure the best possible outcomes. Support from family, friends, and support groups can also play a significant role in coping with the diagnosis and navigating the journey ahead.Future Directions in Group B Strep Research

Advancements in Diagnostic Techniques
Advancements in diagnostic techniques are critical for the early detection and management of Group B strep. Rapid diagnostic tests that can quickly identify the presence of GBS are being developed, allowing for more timely interventions. These advancements not only improve the accuracy of diagnoses but also enable healthcare providers to make informed decisions about treatment, reducing the risk of complications and improving patient outcomes.Conclusion and Final Thoughts

We invite you to share your thoughts and experiences with Group B strep in the comments below. Your insights can help others navigate their journey with GBS, and together, we can foster a community of support and understanding. If you found this article informative, please consider sharing it with others who may benefit from this knowledge.
What is Group B strep, and how common is it?
+Group B strep is a type of bacteria that can be found in the digestive and urinary tracts of adults. It is relatively common, with approximately 25% of healthy adults colonized with GBS.
How is Group B strep transmitted to newborns?
+GBS can be transmitted to newborns during delivery, as they pass through the birth canal. This is why pregnant women who test positive for GBS are given antibiotics during labor to reduce the risk of transmission.
What are the symptoms of Group B strep infection in newborns?
+Symptoms of GBS infection in newborns can include fever, difficulty breathing, lethargy, and poor feeding. In severe cases, GBS can cause pneumonia, meningitis, or sepsis. If you suspect your newborn has contracted GBS, seek medical attention immediately.
