Intro
Learn about Strep B test in pregnancy, including Group B strep screening, symptoms, and treatment to prevent transmission to newborns, ensuring a healthy pregnancy and baby.
Pregnancy is a critical period in a woman's life, filled with excitement, anticipation, and a multitude of changes. As the body prepares to nurture a growing fetus, it's essential to monitor health closely to ensure the well-being of both mother and baby. One crucial aspect of prenatal care is the screening for Group B streptococcus (GBS), commonly referred to as Strep B. This bacterium is naturally found in the digestive tract and lower genital tract of many adults, but it can pose significant risks to newborns if transmitted during birth. Understanding the importance of the Strep B test in pregnancy is vital for expectant mothers to make informed decisions about their care.
The Strep B test is a routine part of prenatal care, typically conducted between 35 and 37 weeks of gestation. The test involves collecting a sample from the vagina and rectum using a swab, which is then sent to a laboratory for analysis. The results indicate whether the mother is a carrier of GBS, which helps healthcare providers determine the best course of action to protect the baby from potential infection. While many women might not exhibit symptoms of GBS colonization, the bacteria can still be present and pose a risk to the newborn. Therefore, the Strep B test is a critical tool in identifying carriers and preventing the transmission of GBS to babies.
The significance of the Strep B test cannot be overstated. GBS infection in newborns can lead to severe illnesses, such as sepsis, pneumonia, and meningitis, which can have long-term consequences or even be fatal. According to the Centers for Disease Control and Prevention (CDC), GBS is a leading cause of illness and death among newborns. However, with proper prenatal care and administration of antibiotics during labor, the risk of transmission can be significantly reduced. This emphasizes the importance of the Strep B test in guiding healthcare decisions and ensuring the best possible outcomes for both mothers and babies.
Understanding Group B Streptococcus
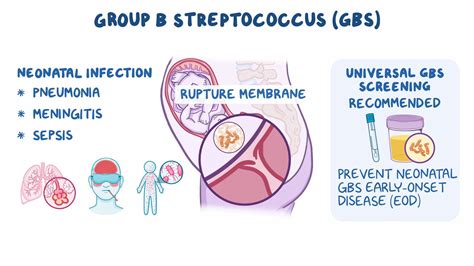
Group B streptococcus is a type of bacteria that can be found in the digestive tract and lower genital tract of adults. It's estimated that approximately 25% of pregnant women are colonized with GBS, although they may not exhibit any symptoms. The bacteria can be transmitted to the baby during vaginal delivery, especially if the mother's water breaks before labor starts. Understanding how GBS is transmitted and the factors that increase the risk of transmission is crucial for developing effective prevention strategies.
Risk Factors for GBS Transmission
Several factors can increase the risk of transmitting GBS to the baby during delivery. These include: - Previous birth of a baby with GBS disease - GBS bacteriuria (presence of GBS in the urine) during pregnancy - Positive GBS culture in the current pregnancy - Labor or rupture of membranes before 37 weeks of gestation - Rupture of membranes for 18 hours or more before delivery - Fever during labor Understanding these risk factors can help healthcare providers identify women who are at higher risk and manage their care accordingly.Strep B Test Procedure
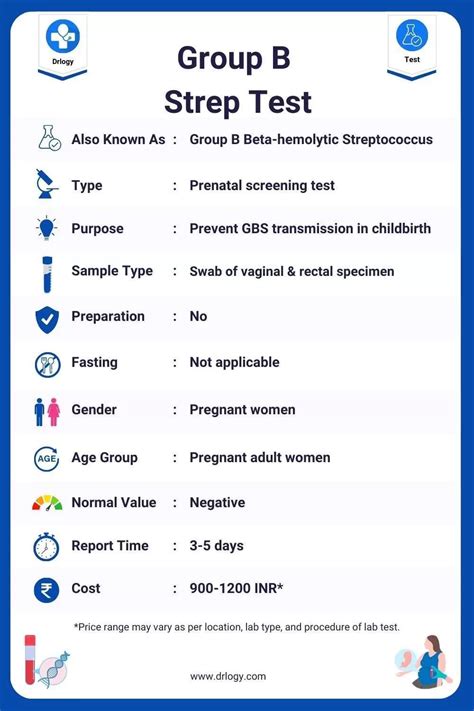
The Strep B test is a straightforward procedure that involves collecting samples from the vagina and rectum using a swab. The sample collection is typically done during a prenatal visit between 35 and 37 weeks of gestation. The swab is then sent to a laboratory for culture, and the results are usually available within a few days. If the test results indicate the presence of GBS, the healthcare provider will discuss the implications and the recommended course of action to prevent transmission to the baby.
Interpreting Test Results
Interpreting the results of the Strep B test is crucial for determining the risk of GBS transmission. A positive test result indicates the presence of GBS in the vagina or rectum, while a negative result suggests that GBS is not present at the time of testing. However, it's essential to note that a negative result does not guarantee that the woman is not a carrier, as the presence of GBS can fluctuate over time. Therefore, even with a negative test result, healthcare providers may still recommend precautions during labor, especially if other risk factors are present.Prevention and Management of GBS
Preventing the transmission of GBS to the baby is a key aspect of prenatal care. For women who test positive for GBS, the administration of intravenous antibiotics during labor is the most effective way to reduce the risk of transmission. The antibiotics work by reducing the amount of GBS bacteria present in the vagina and rectum, thereby decreasing the likelihood of the baby coming into contact with the bacteria during delivery. In addition to antibiotic therapy, other management strategies may include closely monitoring the mother and baby during labor and after birth for signs of infection.
Antibiotic Therapy During Labor
The use of antibiotics during labor is a critical component of GBS prevention. Penicillin is the most commonly recommended antibiotic, although other options may be considered for women who are allergic to penicillin. The antibiotics are administered intravenously, typically starting at least 4 hours before delivery, to ensure that the bacteria are adequately reduced. This approach has been shown to significantly decrease the risk of early-onset GBS disease in newborns.Implications for Pregnancy and Childbirth
The presence of GBS during pregnancy can have significant implications for both the mother and the baby. For mothers who test positive, the primary concern is the risk of transmitting the bacteria to the baby during delivery. This can lead to severe infections in the newborn, which may require prolonged hospital stays and intensive medical care. Understanding these implications can help expectant mothers and their healthcare providers make informed decisions about prenatal care and delivery options.
Delivery Options and GBS
For women who are GBS positive, the mode of delivery does not significantly impact the risk of transmission. However, in certain situations, such as if the mother's water breaks before labor starts or if she has a fever during labor, a cesarean delivery might be recommended to reduce the risk of transmission. It's essential for expectant mothers to discuss their individual circumstances and the best delivery options with their healthcare provider.Support and Resources for Expectant Mothers
Expectant mothers who test positive for GBS or are concerned about the risk of transmission to their baby can find support and resources through various channels. Healthcare providers are an excellent source of information and can address specific questions and concerns. Additionally, numerous online resources, support groups, and educational materials are available to help expectant mothers understand GBS, its implications, and the preventive measures that can be taken.
Coping with a GBS Diagnosis
Receiving a positive GBS test result can be concerning for expectant mothers. However, with the right information and support, women can feel empowered to make informed decisions about their care. It's essential to remember that GBS is a common condition and that effective preventive measures are available. By understanding the risks and the steps that can be taken to mitigate them, expectant mothers can focus on a healthy pregnancy and a positive birth experience.Conclusion and Next Steps

In conclusion, the Strep B test is a vital component of prenatal care, enabling healthcare providers to identify women who are at risk of transmitting GBS to their babies. By understanding the risks associated with GBS and the preventive measures that can be taken, expectant mothers can play an active role in ensuring the best possible outcomes for their babies. Whether through antibiotic therapy during labor or other management strategies, there are effective ways to reduce the risk of GBS transmission. As expectant mothers navigate their pregnancy journey, staying informed and working closely with their healthcare providers are key to a healthy and successful pregnancy.
Final Thoughts
The journey through pregnancy is filled with numerous decisions and considerations. For expectant mothers, being informed about potential risks such as GBS and taking proactive steps to manage them can make a significant difference. By prioritizing prenatal care, including the Strep B test, women can help ensure a healthy start for their babies. As we move forward, continued education, support, and advancements in prenatal care will remain essential in addressing the challenges posed by GBS and other conditions that may affect pregnancy and childbirth.What is Group B streptococcus?
+Group B streptococcus (GBS) is a type of bacteria that can be found in the digestive tract and lower genital tract of adults. It's a common condition, but it can pose significant risks to newborns if transmitted during birth.
Why is the Strep B test important during pregnancy?
+The Strep B test is crucial because it helps identify women who are carriers of GBS, allowing healthcare providers to take preventive measures to reduce the risk of transmission to the baby during delivery.
What happens if I test positive for GBS during pregnancy?
+If you test positive for GBS, your healthcare provider will discuss the implications and recommend the administration of antibiotics during labor to reduce the risk of transmitting GBS to your baby.
We invite you to share your thoughts and experiences regarding the Strep B test and GBS prevention during pregnancy. Your insights can help others better understand the importance of prenatal care and the steps that can be taken to ensure a healthy pregnancy and childbirth experience. Please feel free to comment below or share this article with others who may benefit from this information. Together, we can promote awareness and support expectant mothers in making informed decisions about their care.
