Intro
The tuberculin skin test (TST) is a widely used diagnostic tool to detect infection with Mycobacterium tuberculosis, the bacterium that causes tuberculosis (TB). The test involves injecting a small amount of tuberculin into the skin, and after 48-72 hours, the skin reaction is measured to determine the presence of TB infection. A positive result can have significant implications for an individual's health and treatment. In this article, we will delve into the world of tuberculin skin test positive results, exploring what they mean, the potential causes, and the subsequent steps that need to be taken.
Tuberculosis is a serious public health concern, affecting millions of people worldwide. The World Health Organization (WHO) estimates that in 2020, there were approximately 10 million new cases of TB, resulting in 1.5 million deaths. The TST is an essential tool in the diagnosis of TB, particularly in high-risk populations such as healthcare workers, individuals with compromised immune systems, and those living in areas with high TB prevalence. A positive TST result can indicate that an individual has been infected with TB, even if they do not exhibit any symptoms.
The TST is not a perfect test, and false-positive results can occur due to various factors, including previous vaccination with the Bacille Calmette-Guérin (BCG) vaccine, exposure to non-tuberculous mycobacteria, or incorrect test administration. However, a positive result is generally considered to be a reliable indicator of TB infection. The test measures the body's immune response to the tuberculin, and a positive reaction suggests that the individual has been exposed to TB in the past.
Understanding Tuberculin Skin Test Positive Results
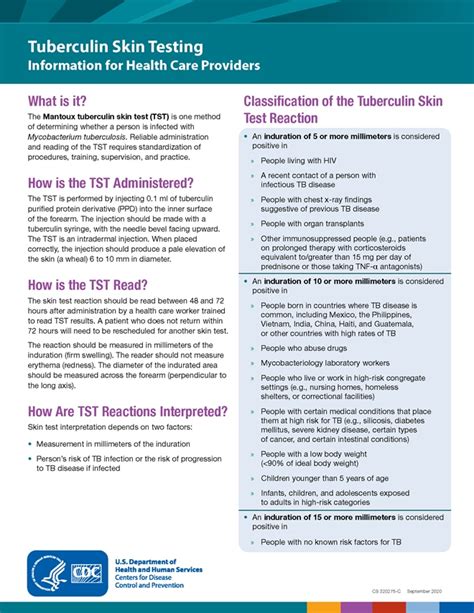
A positive TST result is typically defined as an induration (firm, raised tissue) of 10mm or more in diameter, although the cutoff value may vary depending on the individual's risk factors and medical history. The test result is interpreted based on the size of the induration, with larger reactions indicating a greater likelihood of TB infection. In general, the larger the induration, the more likely it is that the individual has been infected with TB.
Causes of Positive Tuberculin Skin Test Results
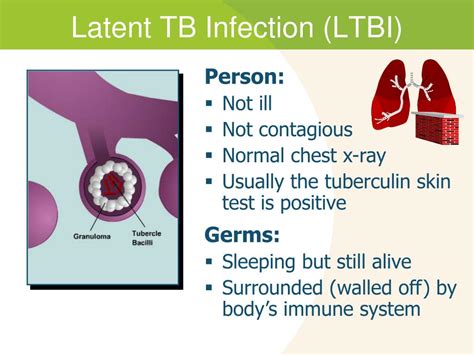
There are several potential causes of a positive TST result, including: * Infection with Mycobacterium tuberculosis * Previous vaccination with the BCG vaccine * Exposure to non-tuberculous mycobacteria * Incorrect test administration * Cross-reactivity with other mycobacteriaIt is essential to note that a positive TST result does not necessarily mean that an individual has active TB disease. In many cases, the infection may be latent, meaning that the bacteria are present in the body but not actively causing disease. Latent TB infection (LTBI) can progress to active TB disease if left untreated, particularly in individuals with compromised immune systems.
Interpretation of Tuberculin Skin Test Results
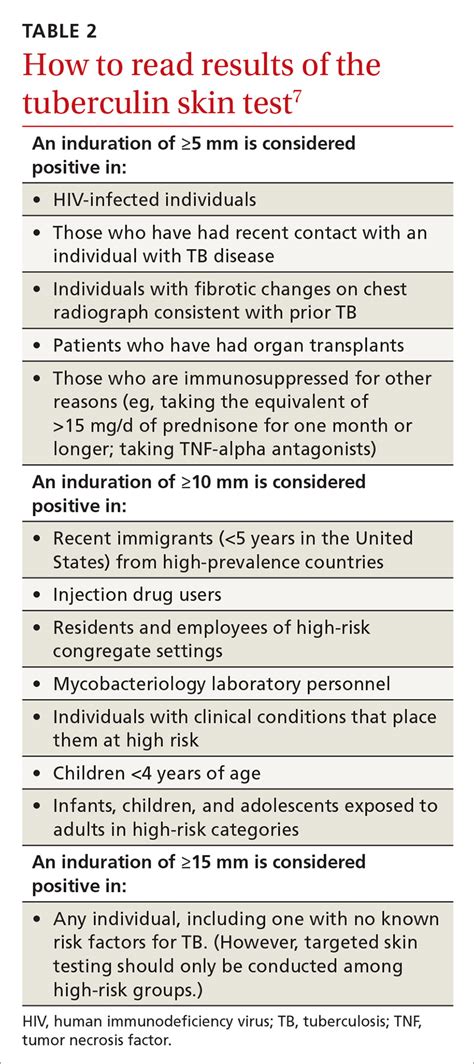
The interpretation of TST results depends on various factors, including the individual's medical history, risk factors, and the size of the induration. The following are general guidelines for interpreting TST results:
- 0-4mm: Negative result, indicating no infection
- 5-9mm: Doubtful result, may require repeat testing
- 10mm or more: Positive result, indicating infection with TB
In individuals with certain medical conditions, such as HIV/AIDS or recent contact with someone with TB, a smaller induration size may be considered positive.
Steps After a Positive Tuberculin Skin Test Result
If an individual receives a positive TST result, the following steps should be taken: 1. **Medical evaluation**: A healthcare provider should evaluate the individual's medical history, perform a physical examination, and order additional tests, such as chest X-rays or sputum tests, to determine if the infection is active or latent. 2. **Treatment**: If the infection is active, the individual will require treatment with anti-TB medications. If the infection is latent, treatment may be recommended to prevent progression to active disease. 3. **Contact tracing**: If the individual has active TB disease, contact tracing may be necessary to identify and test individuals who may have been exposed to the bacteria. 4. **Follow-up care**: Regular follow-up appointments with a healthcare provider are essential to monitor the individual's response to treatment and ensure that the infection is under control.Treatment Options for Latent Tuberculosis Infection
Treatment options for LTBI typically involve a combination of medications, including:
- Isoniazid (INH) monotherapy for 6-9 months
- Rifampin (RIF) monotherapy for 4-6 months
- Combination therapy with INH and RIF for 3-4 months
The choice of treatment regimen depends on various factors, including the individual's medical history, age, and potential drug interactions.
Benefits and Risks of Treatment for Latent Tuberculosis Infection
Treatment for LTBI has several benefits, including: * Reduced risk of progression to active TB disease * Prevention of transmission to others * Reduced risk of TB-related complications, such as meningitis or spinal TBHowever, treatment for LTBI also carries potential risks, including:
- Hepatotoxicity (liver damage) associated with INH and RIF
- Gastrointestinal side effects, such as nausea and vomiting
- Potential interactions with other medications
It is essential to carefully weigh the benefits and risks of treatment and discuss any concerns with a healthcare provider.
Prevention and Control of Tuberculosis
Prevention and control of TB involve a multi-faceted approach, including:
- Vaccination: The BCG vaccine is widely used in high-risk populations to prevent TB.
- Screening: Regular screening of high-risk populations, such as healthcare workers and individuals with compromised immune systems, can help detect TB infection early.
- Infection control: Implementing infection control measures, such as isolation and respiratory protection, can help prevent transmission of TB in healthcare settings.
- Public health initiatives: Public health initiatives, such as contact tracing and outbreak investigations, can help identify and contain TB outbreaks.
Global Efforts to Control Tuberculosis
The WHO has launched several initiatives to control TB, including: * The End TB Strategy, which aims to reduce TB incidence and mortality by 90% by 2035 * The Global Fund to Fight AIDS, Tuberculosis and Malaria, which provides funding for TB control programs in low- and middle-income countries * The Stop TB Partnership, which brings together governments, civil society, and private sector organizations to support TB control effortsThese initiatives have helped to reduce TB incidence and mortality globally, but more work is needed to achieve the goal of a TB-free world.
What is the significance of a positive tuberculin skin test result?
+A positive tuberculin skin test result indicates that an individual has been infected with Mycobacterium tuberculosis, the bacterium that causes tuberculosis.
What are the potential causes of a positive tuberculin skin test result?
+Potential causes of a positive TST result include infection with Mycobacterium tuberculosis, previous vaccination with the BCG vaccine, exposure to non-tuberculous mycobacteria, incorrect test administration, and cross-reactivity with other mycobacteria.
What are the treatment options for latent tuberculosis infection?
+Treatment options for latent tuberculosis infection typically involve a combination of medications, including isoniazid monotherapy, rifampin monotherapy, or combination therapy with isoniazid and rifampin.
In conclusion, a positive tuberculin skin test result can have significant implications for an individual's health and treatment. It is essential to understand the causes and interpretation of TST results, as well as the subsequent steps that need to be taken. By working together to prevent and control TB, we can reduce the burden of this disease and achieve the goal of a TB-free world. We invite you to share your thoughts and experiences with TB, and to join the global effort to control this devastating disease.
