Intro
Discover if Tylenol is safe for pregnant women, exploring its effects on fetus health, dosage guidelines, and alternative pain relief options during pregnancy, ensuring a healthy gestation period.
Pregnancy is a critical period in a woman's life, and it's essential to take care of her health to ensure the well-being of both the mother and the baby. One of the most common health concerns during pregnancy is managing pain and reducing fever. Many pregnant women rely on over-the-counter medications like Tylenol to alleviate their symptoms. However, the safety of Tylenol for pregnant women has been a topic of debate among medical professionals and expectant mothers. In this article, we will delve into the world of Tylenol and its effects on pregnant women, exploring the benefits, risks, and guidelines for safe use.
Pregnancy is a time of significant physical and emotional changes, and it's not uncommon for women to experience headaches, back pain, and fever. While some women may opt for natural remedies like rest, hydration, and relaxation techniques, others may require medication to manage their symptoms. Tylenol, also known as acetaminophen, is a popular pain reliever and fever reducer that has been widely used for decades. Its widespread use during pregnancy has raised concerns about its potential impact on the developing fetus and the mother's health.
The use of Tylenol during pregnancy is a complex issue, and medical professionals have varying opinions on its safety. Some studies suggest that Tylenol is safe for pregnant women when used in moderation, while others raise concerns about its potential risks. The FDA has classified Tylenol as a category B medication, which means that animal studies have shown no fetal risk, but there are no adequate and well-controlled studies in pregnant women. This classification can be misleading, as it may imply that Tylenol is completely safe for pregnant women, when in fact, more research is needed to fully understand its effects.
Tylenol and Pregnancy: Benefits and Risks

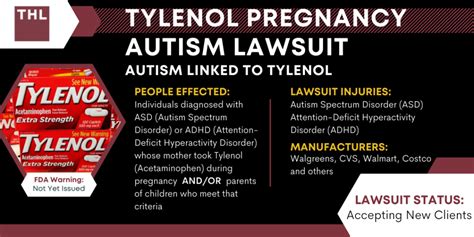
Tylenol can be beneficial for pregnant women when used to relieve pain and reduce fever. It is often recommended as a first-line treatment for headaches, back pain, and other minor ailments. However, its use during pregnancy is not without risks. Some studies have suggested that taking Tylenol during pregnancy may increase the risk of certain health problems, such as asthma, attention deficit hyperactivity disorder (ADHD), and autism spectrum disorder (ASD). Additionally, high doses of Tylenol can cause liver damage and other complications in both the mother and the fetus.
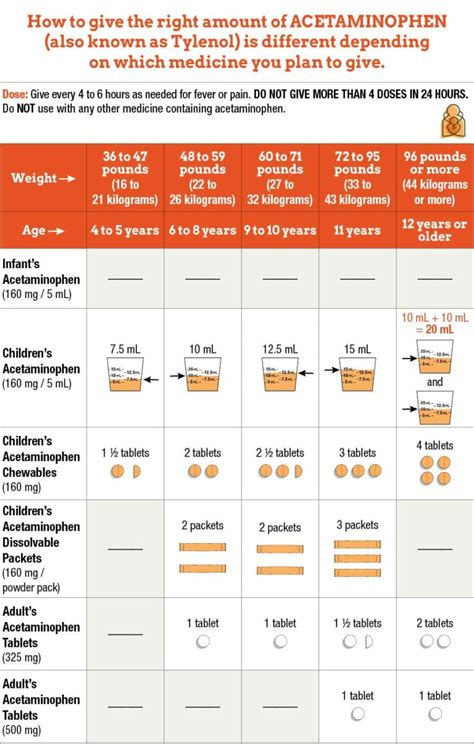
Guidelines for Safe Use
To minimize the risks associated with Tylenol use during pregnancy, it's essential to follow guidelines for safe use. The American College of Obstetricians and Gynecologists (ACOG) recommends that pregnant women use Tylenol only when necessary and in the lowest effective dose. Women should not exceed the recommended dose of 4000mg per day and should avoid taking Tylenol for extended periods. It's also crucial to consult with a healthcare provider before taking Tylenol, especially if you have a pre-existing medical condition or are taking other medications.Tylenol Alternatives for Pregnant Women

While Tylenol may be a convenient option for pain relief, there are alternative remedies that pregnant women can consider. Some natural alternatives include:
- Rest and relaxation techniques, such as meditation and deep breathing
- Heat and cold therapy, such as warm baths and cold compresses
- Gentle exercise, such as prenatal yoga and swimming
- Herbal remedies, such as ginger and chamomile tea
- Acupuncture and massage therapy
These alternatives may not be as effective as Tylenol for severe pain, but they can help alleviate mild to moderate symptoms. It's essential to consult with a healthcare provider before trying any new remedies, especially if you have a pre-existing medical condition or are taking other medications.
Precautions and Warnings
Pregnant women should be aware of the potential risks and precautions associated with Tylenol use. Some precautions include: * Avoiding Tylenol use during the first trimester, when the fetus is most vulnerable to potential harm * Not exceeding the recommended dose of 4000mg per day * Avoiding Tylenol use for extended periods * Consulting with a healthcare provider before taking Tylenol, especially if you have a pre-existing medical condition or are taking other medications * Monitoring liver function and reporting any signs of liver damage, such as nausea, vomiting, and abdominal painTylenol and Fetal Development
The use of Tylenol during pregnancy has raised concerns about its potential impact on fetal development. Some studies have suggested that Tylenol may affect fetal brain development, leading to an increased risk of autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD). However, more research is needed to fully understand the effects of Tylenol on fetal development.
Research and Studies
Several studies have investigated the effects of Tylenol on fetal development. A 2018 study published in the International Journal of Epidemiology found that prenatal exposure to Tylenol was associated with an increased risk of ASD and ADHD. Another study published in the Journal of the American Medical Association (JAMA) in 2019 found that Tylenol use during pregnancy was linked to an increased risk of liver damage in newborns. However, more research is needed to confirm these findings and fully understand the effects of Tylenol on fetal development.Tylenol and Pregnancy Complications
The use of Tylenol during pregnancy has been linked to an increased risk of certain pregnancy complications, such as preterm labor, low birth weight, and preeclampsia. A 2020 study published in the American Journal of Obstetrics and Gynecology found that Tylenol use during pregnancy was associated with an increased risk of preterm labor and low birth weight. Another study published in the Journal of Maternal-Fetal Medicine in 2019 found that Tylenol use during pregnancy was linked to an increased risk of preeclampsia.
Risk Factors and Prevention
Pregnant women can take steps to minimize the risks associated with Tylenol use during pregnancy. Some risk factors include: * Pre-existing medical conditions, such as liver disease or kidney disease * Taking other medications, such as blood thinners or antidepressants * Having a history of pregnancy complications, such as preterm labor or preeclampsia * Using Tylenol for extended periods or exceeding the recommended doseTo prevent pregnancy complications, pregnant women should:
- Consult with a healthcare provider before taking Tylenol
- Follow the recommended dose and duration of use
- Monitor their health and report any signs of complications, such as vaginal bleeding or severe abdominal pain
- Attend regular prenatal appointments to monitor fetal development and health
Conclusion and Recommendations
In conclusion, while Tylenol may be a convenient option for pain relief during pregnancy, its use should be approached with caution. Pregnant women should consult with a healthcare provider before taking Tylenol and follow the recommended dose and duration of use. Alternative remedies, such as natural therapies and lifestyle changes, can also help alleviate symptoms. By understanding the benefits and risks of Tylenol use during pregnancy, women can make informed decisions about their health and the health of their baby.
Final Thoughts
Pregnancy is a unique and critical period in a woman's life, and it's essential to prioritize health and well-being. While Tylenol may be a useful medication for pain relief, its use during pregnancy should be carefully considered. By following guidelines for safe use, consulting with a healthcare provider, and exploring alternative remedies, pregnant women can minimize the risks associated with Tylenol use and ensure a healthy pregnancy.Is Tylenol safe for pregnant women?
+Tylenol can be safe for pregnant women when used in moderation and under the guidance of a healthcare provider. However, its use should be approached with caution, and women should be aware of the potential risks and precautions.
What are the risks of taking Tylenol during pregnancy?
+The risks of taking Tylenol during pregnancy include liver damage, fetal development problems, and pregnancy complications, such as preterm labor and preeclampsia.
Can I take Tylenol during the first trimester?
+It's recommended to avoid Tylenol use during the first trimester, when the fetus is most vulnerable to potential harm. However, if you need to take Tylenol, consult with a healthcare provider to discuss the risks and benefits.
What are some alternative remedies for pain relief during pregnancy?
+Alternative remedies for pain relief during pregnancy include natural therapies, such as rest, hydration, and relaxation techniques, as well as lifestyle changes, such as gentle exercise and heat and cold therapy.
How can I minimize the risks associated with Tylenol use during pregnancy?
+To minimize the risks associated with Tylenol use during pregnancy, follow the recommended dose and duration of use, consult with a healthcare provider, and monitor your health and report any signs of complications.
We hope this article has provided you with valuable information about Tylenol use during pregnancy. If you have any further questions or concerns, please don't hesitate to comment below. Share this article with your friends and family to help spread awareness about the importance of prioritizing health and well-being during pregnancy. Take the first step towards a healthy pregnancy by consulting with a healthcare provider and exploring alternative remedies for pain relief.
