Intro
Upper GI tract hemorrhage symptoms include vomiting blood, black stools, and abdominal pain, indicating a potentially life-threatening condition requiring immediate medical attention for diagnosis and treatment.
Upper gastrointestinal tract hemorrhage, also known as upper GI bleeding, is a serious medical condition that requires immediate attention. The upper GI tract includes the esophagus, stomach, and the first part of the small intestine, known as the duodenum. Bleeding in this area can be life-threatening and necessitates prompt diagnosis and treatment. Understanding the symptoms of upper GI tract hemorrhage is crucial for early detection and intervention.
The symptoms of upper GI bleeding can vary in severity and may develop suddenly or gradually over time. One of the most common and recognizable symptoms is hematemesis, which is the vomiting of blood or material that resembles coffee grounds. This occurs when the blood is partially digested by the stomach acids, giving it a characteristic dark brown or black color. Another symptom is melena, which refers to the passage of black, tarry stools. This happens when the blood is fully digested and passes through the intestines, resulting in stools that are black and sticky.
Other symptoms of upper GI tract hemorrhage may include abdominal pain, nausea, vomiting (not necessarily of blood), and a feeling of weakness or fatigue. In severe cases, patients may experience dizziness, fainting, or shortness of breath due to significant blood loss. It's essential to recognize these symptoms early to prevent complications and improve outcomes.
Causes and Risk Factors

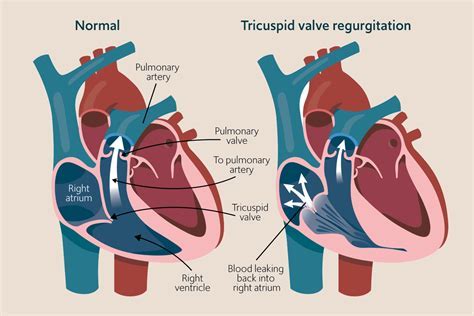
Upper GI tract hemorrhage can be caused by various factors, including peptic ulcers, esophageal varices, gastritis, and Mallory-Weiss syndrome. Peptic ulcers are sores that develop on the inside lining of the stomach and the upper portion of the small intestine, and they are the most common cause of upper GI bleeding. Esophageal varices are enlarged veins in the esophagus, often a result of liver disease, which can rupture and bleed. Gastritis refers to the inflammation of the stomach lining, which can lead to bleeding, and Mallory-Weiss syndrome involves tears in the mucous membrane or lining of the lower end of the esophagus, where it connects to the stomach.
Certain risk factors can increase the likelihood of developing upper GI tract hemorrhage. These include a history of peptic ulcers or gastrointestinal bleeding, use of nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, or anticoagulant medications, liver disease, and heavy alcohol consumption. Age is also a risk factor, with the incidence of upper GI bleeding increasing significantly after the age of 60.
Diagnosis and Evaluation
Diagnosing upper GI tract hemorrhage involves a combination of clinical evaluation, laboratory tests, and endoscopic procedures. The initial assessment includes a thorough medical history, physical examination, and laboratory tests such as complete blood count (CBC), blood urea nitrogen (BUN), creatinine, and liver function tests to evaluate the extent of blood loss and potential underlying causes.
Endoscopy is a critical diagnostic tool for upper GI bleeding, allowing direct visualization of the esophagus, stomach, and duodenum. It can identify the source of bleeding, such as ulcers, varices, or erosions, and in many cases, treatment can be administered during the procedure to stop the bleeding. Other imaging studies like computed tomography (CT) scans may be used in certain situations to evaluate for other potential causes of bleeding.
Endoscopic Techniques
Endoscopic techniques play a pivotal role in the management of upper GI tract hemorrhage. These techniques not only help in diagnosing the cause of bleeding but also in providing therapeutic interventions. Common endoscopic treatments include the application of clips, thermal coagulation, and injection of vasoconstrictor agents or sclerosing agents to control bleeding.Treatment and Management
The treatment of upper GI tract hemorrhage is multifaceted and depends on the underlying cause, severity of bleeding, and the patient's overall health status. Initial management involves stabilizing the patient with fluid resuscitation and blood transfusions as needed. Medications such as proton pump inhibitors (PPIs) are often administered to reduce stomach acid and promote healing of ulcers or erosions.
Endoscopic therapy, as mentioned earlier, is a cornerstone in the treatment of upper GI bleeding, especially for bleeding ulcers and varices. For cases where endoscopic treatment is not feasible or unsuccessful, interventional radiology procedures like angiographic embolization may be considered to control bleeding. In some instances, surgery may be necessary, especially if there is a high risk of rebleeding or if endoscopic and radiologic interventions are not possible.
Prevention Strategies
Preventing upper GI tract hemorrhage is crucial, especially in high-risk individuals. Strategies include the use of protective medications like PPIs for patients on long-term NSAID or aspirin therapy, avoiding heavy alcohol consumption, and managing liver disease. Regular monitoring and follow-up with healthcare providers are also essential for early detection and treatment of potential causes of upper GI bleeding.Complications and Prognosis
The prognosis of upper GI tract hemorrhage depends on several factors, including the severity of bleeding, underlying cause, patient's age, and presence of comorbid conditions. Complications can arise from both the bleeding itself and the treatment modalities. Significant blood loss can lead to shock, organ failure, and even death. Rebleeding is a significant concern, especially in the first few days after the initial bleed, and can impact outcomes.
Understanding the potential complications and being aware of the signs of rebleeding or worsening condition can help in early intervention and improvement of prognosis. Follow-up care and adherence to treatment plans are crucial for preventing recurrence and managing underlying conditions that may have contributed to the upper GI tract hemorrhage.
Current Research and Advances
Research into upper GI tract hemorrhage is ongoing, focusing on improving diagnostic techniques, developing more effective treatments, and exploring preventive strategies. Advances in endoscopic technology and interventional radiology have significantly improved the management of upper GI bleeding. Furthermore, studies on the pharmacological prevention of rebleeding and the role of novel anticoagulants in patients with upper GI bleeding are providing new insights into the management of this condition.
The development of scoring systems to predict the risk of rebleeding and death has also been an area of interest, helping clinicians to stratify patients according to their risk and tailor management strategies accordingly. As our understanding of the pathophysiology and risk factors associated with upper GI tract hemorrhage evolves, so too will the approaches to its prevention and treatment.
Conclusion and Future Directions
In conclusion, upper GI tract hemorrhage is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and effective treatment. The management of upper GI bleeding involves a multidisciplinary approach, incorporating medical, endoscopic, and sometimes surgical interventions. As research continues to uncover the intricacies of this condition and novel therapeutic strategies are developed, the prognosis for patients with upper GI tract hemorrhage is expected to improve.
It is essential for healthcare providers and patients alike to be aware of the risk factors, symptoms, and latest management strategies for upper GI bleeding. By fostering a collaborative approach to patient care and staying abreast of the latest advances in the field, we can work towards reducing the morbidity and mortality associated with this condition.
What are the common symptoms of upper GI tract hemorrhage?
+The common symptoms include vomiting blood or coffee ground-like material, black tarry stools, abdominal pain, nausea, and a feeling of weakness or fatigue.
What are the main causes of upper GI tract hemorrhage?
+The main causes include peptic ulcers, esophageal varices, gastritis, and Mallory-Weiss syndrome.
How is upper GI tract hemorrhage diagnosed?
+Diagnosis involves a combination of clinical evaluation, laboratory tests, and endoscopic procedures to identify the source of bleeding and evaluate the extent of blood loss.
What are the treatment options for upper GI tract hemorrhage?
+Treatment options include fluid resuscitation, blood transfusions, medications to reduce stomach acid, endoscopic therapy to control bleeding, and in some cases, surgery or interventional radiology procedures.
How can upper GI tract hemorrhage be prevented?
+Prevention strategies include the use of protective medications for patients on long-term NSAID or aspirin therapy, avoiding heavy alcohol consumption, managing liver disease, and regular monitoring and follow-up with healthcare providers.
We invite you to share your thoughts and experiences regarding upper GI tract hemorrhage. Your insights can help others understand this complex condition better and may provide valuable perspectives on its management and prevention. Please feel free to comment, share this article with those who may benefit from it, and engage in discussions that can lead to improved patient outcomes and advancements in the field of gastroenterology.
