Intro
Discover causes, symptoms, and treatments for varicose veins during pregnancy, including spider veins, swollen legs, and relief methods to alleviate discomfort and promote healthy blood flow.
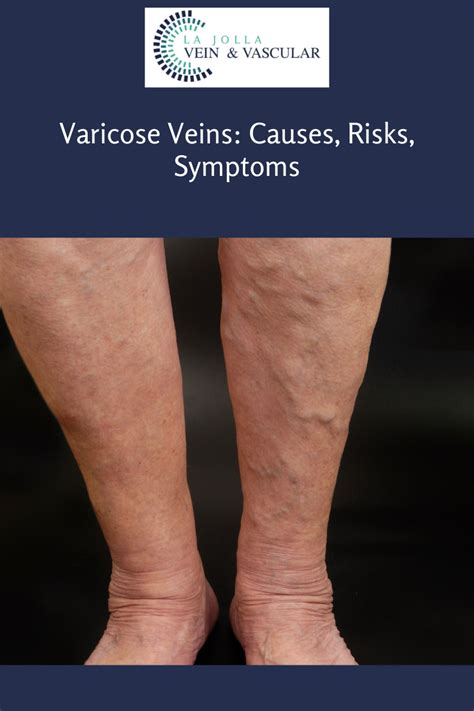
Pregnancy is a unique and transformative experience for women, marked by significant physical, emotional, and hormonal changes. Among the various symptoms and discomforts that women may encounter during pregnancy, varicose veins are a common issue that can cause concern and discomfort. Varicose veins are enlarged, twisted veins that can appear on the surface of the skin, often on the legs, and are more prevalent during pregnancy due to increased blood volume and pressure on the veins. Understanding the causes, symptoms, and treatment options for varicose veins during pregnancy is essential for managing this condition and ensuring a healthy pregnancy.
The development of varicose veins during pregnancy can be attributed to several factors, including the increased blood volume that occurs to support the growing fetus, hormonal changes that relax the blood vessel walls, and the pressure exerted by the expanding uterus on the pelvic veins. These factors can lead to the pooling of blood in the veins, causing them to swell and become varicose. While varicose veins can be unsightly and uncomfortable, they are generally not a cause for concern and often resolve on their own after pregnancy. However, in some cases, varicose veins can lead to more serious complications, such as blood clots or ulcers, which require prompt medical attention.
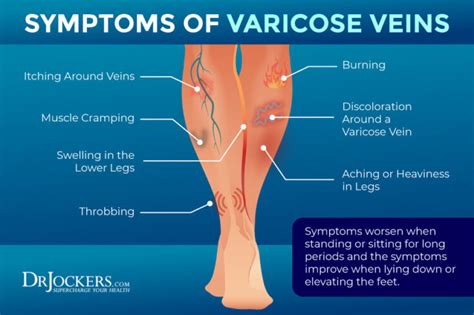
The symptoms of varicose veins during pregnancy can vary from woman to woman but often include visible, bulging veins on the surface of the skin, aching or heaviness in the legs, swelling in the feet and ankles, and itching or burning sensations around the affected veins. In some cases, varicose veins can also lead to more severe symptoms, such as pain or discomfort during physical activity, skin discoloration or ulcers, and a feeling of fatigue or restlessness in the legs. If left untreated, varicose veins can significantly impact a woman's quality of life during pregnancy, making it essential to seek medical attention if symptoms persist or worsen over time.
Causes and Risk Factors
Genetic Predisposition
Genetic predisposition is a significant risk factor for varicose veins during pregnancy, with women who have a family history of varicose veins being more likely to develop them. This is because genetic factors can affect the structure and function of the blood vessels, making them more susceptible to damage and dysfunction. Women with a family history of varicose veins should take preventive measures, such as maintaining a healthy weight, exercising regularly, and avoiding prolonged standing or sitting.Hormonal Changes
Hormonal changes during pregnancy, such as the increased levels of progesterone, can cause the blood vessel walls to relax, leading to the pooling of blood in the veins. Progesterone can also affect the blood's ability to clot, increasing the risk of blood clots and other complications. Understanding the impact of hormonal changes on varicose veins can help women take preventive measures, such as wearing compression stockings or elevating their legs regularly.Symptoms and Diagnosis
Physical Examination
A physical examination is often the first step in diagnosing varicose veins during pregnancy. During the examination, the healthcare provider will look for visible signs of varicose veins, such as bulging or twisted veins, and assess the woman's overall health and medical history. The healthcare provider may also perform a series of tests, such as checking the blood flow in the legs or looking for signs of swelling or skin discoloration.Imaging Tests
Imaging tests, such as ultrasound or Doppler studies, may be used to confirm the diagnosis of varicose veins and rule out other conditions. These tests can help the healthcare provider visualize the blood flow in the veins and assess the severity of the varicose veins. In some cases, imaging tests may also be used to monitor the progression of varicose veins during pregnancy and adjust treatment plans accordingly.Treatment Options

Self-Care Measures
Self-care measures can play a significant role in managing varicose veins during pregnancy. Elevating the legs regularly, avoiding prolonged standing or sitting, and wearing compression stockings can help reduce swelling and alleviate symptoms. Additionally, maintaining a healthy weight, exercising regularly, and avoiding tight clothing can also help reduce the risk of developing varicose veins.Medical Treatments
Medical treatments, such as sclerotherapy or endovenous laser therapy, may be necessary to close or remove the affected veins. These treatments are typically performed under local anesthesia and can be effective in reducing symptoms and improving appearance. However, medical treatments may not be suitable for all women, particularly those with severe varicose veins or underlying medical conditions.Prevention and Management

Lifestyle Changes
Lifestyle changes, such as maintaining a healthy weight, exercising regularly, and avoiding prolonged standing or sitting, can help reduce the risk of developing varicose veins. Additionally, avoiding tight clothing, elevating the legs regularly, and wearing compression stockings can also help alleviate symptoms and improve appearance.Medical Follow-Up
Medical follow-up is essential for managing varicose veins during pregnancy. Regular check-ups with a healthcare provider can help monitor the progression of varicose veins and adjust treatment plans accordingly. Additionally, medical follow-up can help identify potential complications, such as blood clots or ulcers, and provide prompt treatment to prevent long-term damage.What are the symptoms of varicose veins during pregnancy?
+The symptoms of varicose veins during pregnancy can include visible, bulging veins on the surface of the skin, aching or heaviness in the legs, swelling in the feet and ankles, and itching or burning sensations around the affected veins.
How can I prevent varicose veins during pregnancy?
+Preventing varicose veins during pregnancy requires a combination of self-care measures, lifestyle changes, and medical treatments. Maintaining a healthy weight, exercising regularly, and avoiding prolonged standing or sitting can help reduce the risk of developing varicose veins.
What are the treatment options for varicose veins during pregnancy?
+The treatment options for varicose veins during pregnancy depend on the severity of the condition and the individual woman's needs. In mild cases, self-care measures, such as elevating the legs and wearing compression stockings, may be sufficient to manage symptoms. In more severe cases, medical treatments, such as sclerotherapy or endovenous laser therapy, may be necessary to close or remove the affected veins.
In conclusion, varicose veins during pregnancy are a common condition that can cause discomfort and concern for women. Understanding the causes, symptoms, and treatment options for varicose veins can help women manage this condition and ensure a healthy pregnancy. By taking preventive measures, such as maintaining a healthy weight, exercising regularly, and avoiding prolonged standing or sitting, women can reduce the risk of developing varicose veins. Additionally, seeking medical attention if symptoms persist or worsen over time can help prevent long-term damage and improve overall health and well-being. We invite you to share your thoughts and experiences with varicose veins during pregnancy in the comments section below. If you found this article helpful, please share it with your friends and family to help raise awareness about this common condition.
