Intro
The importance of understanding and addressing healthcare-associated infections (HAIs) cannot be overstated. Among the various types of HAIs, one that has garnered significant attention in recent years is Vancomycin-Resistant Enterococci (VRE). The emergence and spread of VRE have posed considerable challenges to healthcare systems worldwide, necessitating a comprehensive approach to prevention, diagnosis, and treatment. As we delve into the world of VRE, it becomes clear that this issue is multifaceted, involving not just medical professionals but also the broader community.
VRE infections have been on the rise, and their impact on patient outcomes and healthcare resource utilization is substantial. The ability of Enterococci to develop resistance to vancomycin, a drug of last resort for many bacterial infections, complicates treatment protocols and underscores the need for stringent infection control measures. Furthermore, the economic burden of VRE infections, including prolonged hospital stays and the need for more expensive treatments, highlights the urgency of addressing this issue effectively.
Understanding VRE requires a nuanced approach, considering its causes, risk factors, and the strategies employed to combat its spread. It is essential to recognize that VRE is not just a medical concern but also a public health issue, with implications for how we manage and prevent infections in various settings. As we explore the complexities of VRE, we will examine its microbiology, epidemiology, clinical manifestations, and the current best practices for its management. This knowledge is crucial for healthcare professionals, patients, and the community at large, as we work together to mitigate the impact of VRE and ensure a safer, healthier environment for everyone.
Introduction to VRE
VRE refers to strains of Enterococci bacteria that have developed resistance to vancomycin, an antibiotic that has been a cornerstone in the treatment of serious bacterial infections. Enterococci are part of the normal flora of the human gastrointestinal tract but can become pathogenic under certain conditions, leading to infections. The resistance to vancomycin complicates the treatment of these infections, as vancomycin is often used as a drug of last resort.
Mechanism of Resistance
The mechanism of resistance in VRE involves alterations in the bacterial cell wall, which reduce the affinity of vancomycin for its target site. This alteration prevents vancomycin from effectively inhibiting cell wall synthesis, thereby allowing the bacteria to survive and multiply despite the presence of the antibiotic.Epidemiology of VRE
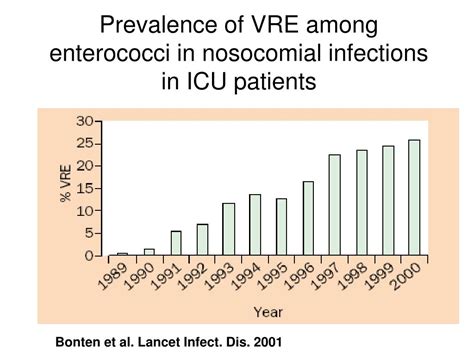
The epidemiology of VRE is complex, involving the spread of resistant strains within healthcare settings and the community. Risk factors for acquiring VRE infections include prolonged hospital stays, exposure to invasive medical devices, and previous use of antibiotics, particularly vancomycin. The spread of VRE is facilitated by inadequate infection control practices, such as poor hand hygiene and insufficient environmental cleaning.
Global Prevalence
The global prevalence of VRE varies, with some regions reporting higher rates of resistance than others. This variability is influenced by factors such as antibiotic use patterns, infection control practices, and the presence of resistant strains in the community.Clinical Manifestations of VRE Infections
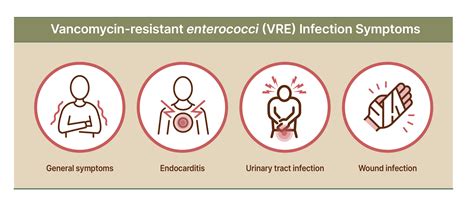
VRE infections can manifest in various ways, including urinary tract infections, bloodstream infections, and wound infections. The clinical presentation of VRE infections does not differ significantly from that of infections caused by susceptible strains, making laboratory diagnosis crucial for guiding treatment.
Diagnosis
The diagnosis of VRE infections relies on microbiological cultures and molecular tests to detect the presence of vancomycin-resistant strains. Prompt diagnosis is essential for initiating appropriate antibiotic therapy and implementing infection control measures to prevent further spread.Management and Treatment of VRE Infections
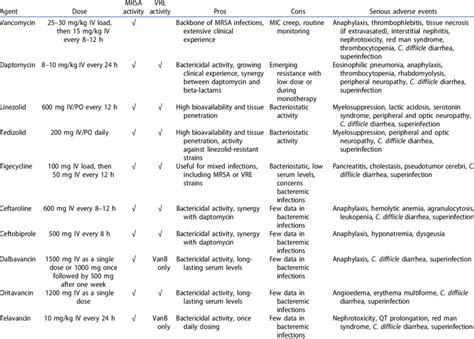
The management of VRE infections involves a multifaceted approach, including the use of alternative antibiotics, infection control measures, and, in some cases, decolonization strategies. The choice of antibiotic therapy depends on the susceptibility pattern of the infecting strain and the site and severity of the infection.
Prevention Strategies
Prevention of VRE infections is critical and involves a range of strategies, including: - Enhanced infection control practices, such as improved hand hygiene and environmental cleaning. - Prudent use of antibiotics to reduce the selective pressure for resistance. - Active surveillance for VRE colonization and infection in high-risk settings. - Implementation of contact precautions for patients known to be colonized or infected with VRE.Future Directions in Combatting VRE

As we look to the future, it is clear that combating VRE will require a sustained effort from healthcare professionals, researchers, and the community. This includes the development of new antibiotics and diagnostic tools, as well as continued emphasis on infection prevention and control. Additionally, addressing the root causes of antibiotic resistance, such as misuse and overuse of antibiotics, is crucial for mitigating the rise of resistant organisms like VRE.
Research and Development
Ongoing research into the mechanisms of resistance, the development of new therapeutic agents, and the improvement of infection control strategies is vital. This research should be complemented by public health initiatives aimed at promoting antibiotic stewardship and reducing the transmission of resistant organisms.Conclusion and Call to Action
In conclusion, VRE represents a significant challenge to healthcare systems worldwide. Addressing this challenge requires a comprehensive approach that includes enhanced infection control practices, prudent use of antibiotics, and ongoing research into new therapeutic strategies. It is imperative that we work together—healthcare professionals, patients, and the community—to mitigate the impact of VRE and ensure a safer, healthier environment for everyone.
We invite you to share your thoughts and experiences related to VRE in the comments section below. Your insights can help foster a deeper understanding of this complex issue and contribute to the development of effective strategies for its management. Furthermore, we encourage you to share this article with others who may be interested in learning more about VRE, as collective knowledge and action are key to addressing the challenges posed by antibiotic-resistant bacteria.
What is VRE?
+VRE stands for Vancomycin-Resistant Enterococci, which are strains of Enterococci bacteria that have developed resistance to the antibiotic vancomycin.
How is VRE spread?
+VRE can be spread through direct contact with an infected person, contaminated surfaces, or through the healthcare environment if proper infection control practices are not followed.
Can VRE infections be treated?
+Yes, VRE infections can be treated with alternative antibiotics, but the choice of antibiotic depends on the susceptibility pattern of the infecting strain and the site and severity of the infection.
