Intro
Understand Alk Phosphatase levels, a key enzyme indicator, and its relation to liver and bone health, including causes of elevated or low levels, symptoms, and diagnostic tests for abnormal Alkaline Phosphatase readings.
Alkaline phosphatase, often abbreviated as ALP, is an enzyme found in various tissues throughout the body. It plays a crucial role in the process of bone mineralization and the breakdown of proteins. Understanding ALP levels is essential for diagnosing and managing certain health conditions. In this article, we will delve into the world of ALP, exploring its functions, the significance of ALP levels, and how they are interpreted in clinical settings.
The importance of monitoring ALP levels cannot be overstated. Elevated or decreased levels of this enzyme can indicate a range of health issues, from bone disorders to liver diseases. Healthcare professionals rely on ALP tests as part of a broader diagnostic approach to identify the underlying causes of symptoms such as bone pain, jaundice, or fatigue. By grasping the fundamentals of ALP and its clinical implications, individuals can better navigate their health care, making informed decisions about their well-being.
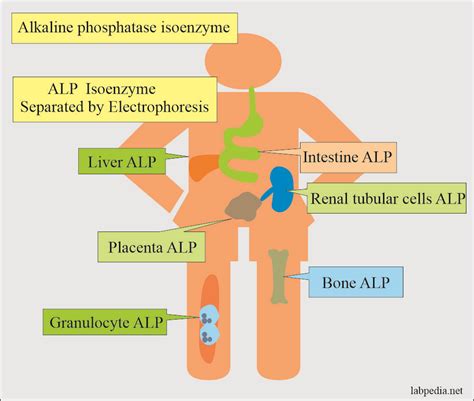
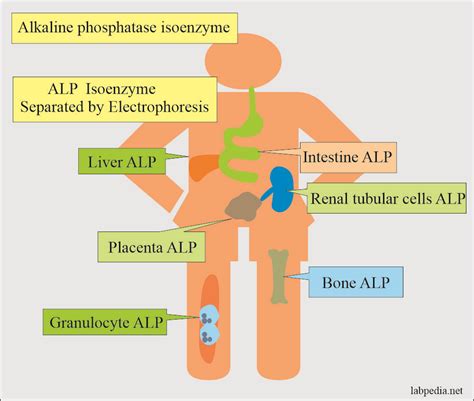
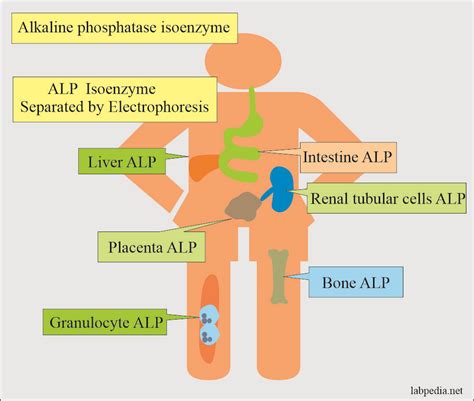
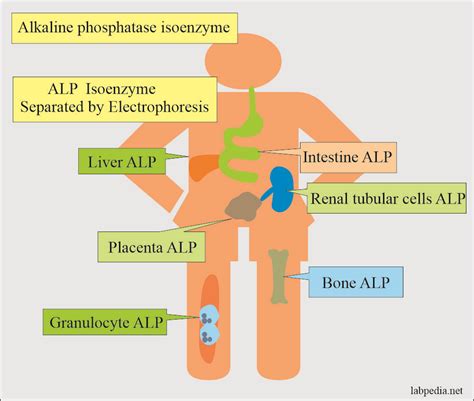
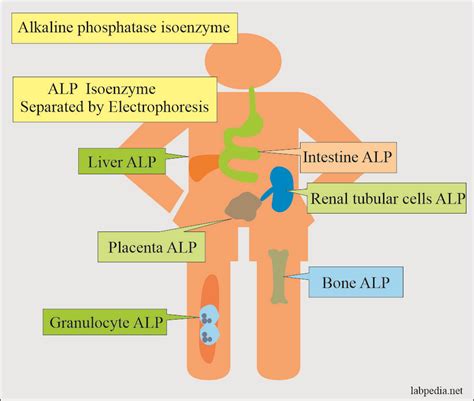
Alkaline phosphatase is not just one enzyme but a group of enzymes that share similar properties and functions. They are primarily found in the liver, bones, kidneys, and digestive system. The liver contains the highest concentrations of ALP, which is why liver diseases often lead to elevated ALP levels in the blood. The bone-specific form of ALP is crucial for the mineralization of bones, making it a key marker for bone health and diseases such as osteomalacia or Paget's disease. Understanding the distribution and functions of ALP in the body is vital for interpreting ALP levels and diagnosing related conditions.
Introduction to Alkaline Phosphatase
Alkaline phosphatase is naturally present in the bloodstream, and its levels can fluctuate based on various factors, including age, sex, and overall health. In adults, the level of ALP tends to be relatively stable, whereas in children and adolescents, ALP levels are typically higher due to bone growth and development. The measurement of ALP levels is usually part of a liver panel or a bone profile, depending on the clinical context. These tests are essential for assessing liver function, bone health, and the presence of certain diseases.
Functions of Alkaline Phosphatase
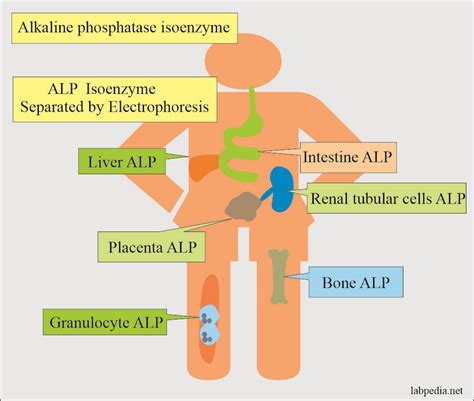
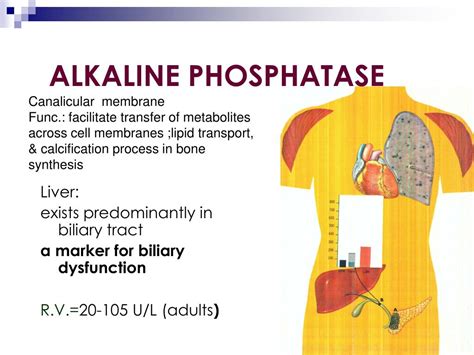
The primary functions of alkaline phosphatase include the removal of phosphate groups from proteins, a process known as dephosphorylation, and the facilitation of bone mineralization. In the liver, ALP plays a role in the transport of lipids and in the metabolism of bile. The enzyme's activity is crucial for maintaining the balance of minerals in the body, particularly calcium and phosphorus, which are vital for bone health. Abnormal ALP levels can signal disruptions in these processes, indicating potential health issues that require medical attention.
Clinical Significance of ALP Levels
The clinical significance of ALP levels lies in their ability to indicate the presence of liver or bone diseases. Elevated ALP levels can be associated with conditions such as hepatitis, cirrhosis, or bone cancer. On the other hand, low ALP levels are less common but can be seen in cases of hypophosphatasia, a rare genetic disorder affecting bone mineralization. The interpretation of ALP levels must be done in conjunction with other clinical findings, including symptoms, medical history, and the results of other diagnostic tests.
Interpretation of ALP Levels
The interpretation of ALP levels involves considering the reference range provided by the laboratory, which can vary slightly depending on the testing method and the population being tested. Generally, ALP levels are considered elevated if they exceed the upper limit of the reference range. The degree of elevation can provide clues about the underlying condition, with significantly higher levels often associated with more severe diseases. It's also important to note that transient elevations in ALP can occur due to non-pathological conditions, such as during pregnancy or in response to certain medications.
Elevated ALP Levels: Causes and Implications
Elevated ALP levels can be caused by a variety of conditions, including liver diseases (like hepatitis or cirrhosis), bone disorders (such as Paget's disease or osteomalacia), and other health issues (including thyroid diseases or certain types of cancer). The clinical implications of elevated ALP levels depend on the underlying cause. For instance, if the elevation is due to liver disease, it may indicate liver damage or dysfunction, which can have significant implications for the patient's health and treatment plan.
Causes of Elevated ALP Levels
Understanding the causes of elevated ALP levels is crucial for developing an effective treatment plan. In some cases, elevated ALP may be a sign of an underlying condition that requires immediate medical attention. For example, if the elevation is due to a liver condition, the patient may need to undergo further testing, such as liver biopsy or imaging studies, to determine the extent of the liver damage. In cases where the elevation is due to bone disease, the patient may require treatment to manage bone health and prevent complications.
Low ALP Levels: Causes and Clinical Significance
Low ALP levels are less common than elevated levels but can be indicative of certain health issues. Hypophosphatasia is a rare genetic disorder characterized by low ALP levels, leading to impaired bone mineralization. Other causes of low ALP levels include malnutrition, particularly deficiencies in zinc or magnesium, which are essential for ALP activity. The clinical significance of low ALP levels depends on the underlying cause and may require specific treatment to address the deficiency or underlying condition.
Low ALP Levels: Diagnosis and Management
The diagnosis and management of low ALP levels involve identifying the underlying cause and implementing appropriate treatment. This may include dietary changes to address nutritional deficiencies or, in the case of hypophosphatasia, specific therapies aimed at managing the condition and preventing complications. The management of low ALP levels requires a comprehensive approach, considering the patient's overall health, medical history, and the presence of any other conditions that may be contributing to the low ALP levels.
ALP Levels in Clinical Practice
In clinical practice, ALP levels are a valuable tool for diagnosing and monitoring a range of conditions. Healthcare providers use ALP tests in conjunction with other diagnostic tools, such as imaging studies and biopsies, to determine the cause of elevated or decreased ALP levels. The interpretation of ALP levels must be done carefully, considering the patient's clinical presentation, medical history, and the results of other tests. By understanding the significance of ALP levels, healthcare providers can develop targeted treatment plans to address the underlying condition and improve patient outcomes.
ALP Levels in Liver Diseases
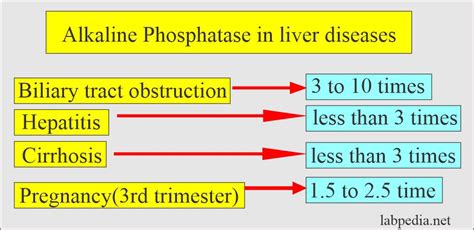
ALP levels are particularly significant in the diagnosis and management of liver diseases. Elevated ALP levels can indicate liver damage or dysfunction, which may be due to a variety of causes, including viral hepatitis, alcoholic liver disease, or cirrhosis. The degree of elevation can provide clues about the severity of the liver condition, and serial measurements of ALP levels can be used to monitor the patient's response to treatment. In some cases, elevated ALP levels may also be associated with liver cancer, highlighting the importance of further diagnostic evaluation in patients with unexplained elevations in ALP.
ALP Levels in Bone Diseases
ALP levels are also crucial in the diagnosis and management of bone diseases. The bone-specific form of ALP is a key marker for bone health, and elevated levels can indicate conditions such as Paget's disease, osteomalacia, or bone cancer. In children and adolescents, elevated ALP levels are common due to bone growth and development, but in adults, such elevations can signal underlying bone pathology. The interpretation of ALP levels in the context of bone diseases requires consideration of the patient's age, sex, and clinical presentation, as well as the results of other diagnostic tests, such as bone density scans or biopsies.
ALP Levels in Other Conditions
ALP levels can be affected by a range of conditions beyond liver and bone diseases. For example, certain thyroid disorders, such as hyperthyroidism, can lead to elevated ALP levels. Similarly, ALP levels may be elevated in patients with kidney disease or certain types of cancer. The clinical significance of ALP levels in these conditions depends on the underlying cause and the patient's overall health status. By understanding the relationship between ALP levels and various health conditions, healthcare providers can use ALP tests as a valuable diagnostic tool to guide patient care.
Limitations and Future Directions
While ALP levels provide valuable information for diagnosing and managing various health conditions, there are limitations to their use. The interpretation of ALP levels can be complex, and elevations can be non-specific, requiring further testing to determine the underlying cause. Future research directions include the development of more specific markers for liver and bone diseases, as well as a better understanding of the molecular mechanisms underlying ALP regulation. By advancing our knowledge of ALP and its role in health and disease, we can improve diagnostic accuracy and develop more effective treatment strategies for patients with elevated or decreased ALP levels.
Conclusion and Recommendations
In conclusion, alkaline phosphatase levels are a critical component of diagnostic testing, providing insights into liver and bone health, among other conditions. Understanding the functions, clinical significance, and interpretation of ALP levels is essential for healthcare providers to make informed decisions about patient care. As research continues to uncover the complexities of ALP regulation and its role in disease, it is likely that our understanding and use of ALP levels will evolve, leading to improved diagnostic accuracy and patient outcomes.
We invite readers to share their thoughts and experiences regarding alkaline phosphatase levels and their role in health and disease. Your comments and questions can help us better understand the complexities of ALP and its significance in clinical practice. By engaging in this discussion, we can work together to advance our knowledge of ALP and improve patient care.
What is the normal range for alkaline phosphatase levels?
+The normal range for alkaline phosphatase (ALP) levels can vary slightly depending on the laboratory and the specific testing method used. Generally, the normal range for adults is between 30 and 120 U/L. However, it's essential to consult with a healthcare provider for the most accurate interpretation of ALP levels, as the reference range may differ.
What causes elevated alkaline phosphatase levels?
+Elevated alkaline phosphatase levels can be caused by a variety of conditions, including liver diseases (such as hepatitis or cirrhosis), bone disorders (like Paget's disease or osteomalacia), and other health issues (including thyroid diseases or certain types of cancer). The degree of elevation can provide clues about the underlying condition.
How are low alkaline phosphatase levels treated?
+The treatment of low alkaline phosphatase levels depends on the underlying cause. In cases of nutritional deficiencies, such as zinc or magnesium deficiency, dietary changes or supplements may be recommended. For conditions like hypophosphatasia, specific therapies aimed at managing the disorder and preventing complications may be necessary. Consultation with a healthcare provider is essential for determining the appropriate treatment plan.
