Intro
Discover the best inflammatory pain drugs, including NSAIDs, corticosteroids, and DMARDs, to relieve arthritis, joint pain, and swelling, and learn about their benefits, side effects, and interactions.
Inflammatory pain is a common condition that affects millions of people worldwide, causing discomfort, stiffness, and limited mobility. The management of inflammatory pain often involves the use of medications, which can provide relief from symptoms and improve quality of life. With numerous options available, it's essential to understand the best inflammatory pain drugs and their mechanisms of action.
Inflammatory pain can result from various conditions, such as arthritis, tendinitis, and bursitis. The pain is typically caused by the activation of inflammatory pathways, which lead to the release of pro-inflammatory mediators, such as cytokines and prostaglandins. These chemicals stimulate nerve endings, transmitting pain signals to the brain. Effective management of inflammatory pain requires a comprehensive approach, including lifestyle modifications, physical therapy, and pharmacological interventions.
The primary goal of inflammatory pain management is to reduce inflammation, alleviate pain, and improve functional ability. Non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are commonly used to treat inflammatory pain. However, other medications, such as biologics and disease-modifying antirheumatic drugs (DMARDs), may also be prescribed, depending on the underlying condition and disease severity.
Inflammatory Pain Mechanisms
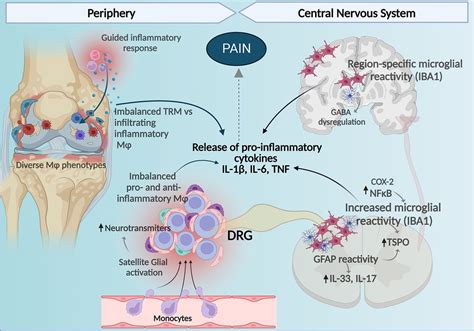
Understanding the mechanisms of inflammatory pain is crucial for developing effective treatment strategies. The inflammatory response involves a complex interplay between various cell types, including immune cells, endothelial cells, and nerve fibers. Pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-1 beta (IL-1β), play a key role in initiating and maintaining the inflammatory response. These cytokines stimulate the production of prostaglandins, which sensitize nerve endings and contribute to pain transmission.
Key Players in Inflammatory Pain
The management of inflammatory pain often involves targeting specific molecules or pathways involved in the inflammatory response. Some key players in inflammatory pain include: * Pro-inflammatory cytokines (e.g., TNF-alpha, IL-1β) * Prostaglandins (e.g., PGE2) * Bradykinin * Histamine * Substance PNon-Steroidal Anti-Inflammatory Drugs (NSAIDs)
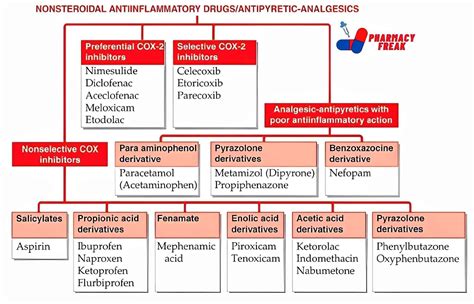
NSAIDs are a class of medications that are widely used to treat inflammatory pain. They work by inhibiting the production of prostaglandins, which are key mediators of inflammation and pain. Commonly used NSAIDs include:
- Ibuprofen
- Naproxen
- Aspirin
- Celecoxib
- Diclofenac
NSAIDs are effective in reducing pain and inflammation, but they can also have gastrointestinal and cardiovascular side effects. The risk of these side effects can be minimized by using the lowest effective dose and taking the medication with food.
COX-2 Inhibitors
COX-2 inhibitors are a subclass of NSAIDs that specifically target the COX-2 enzyme, which is involved in the production of prostaglandins. Examples of COX-2 inhibitors include: * Celecoxib * Rofecoxib (withdrawn from the market due to safety concerns) * Valdecoxib (withdrawn from the market due to safety concerns)COX-2 inhibitors have a lower risk of gastrointestinal side effects compared to traditional NSAIDs but may increase the risk of cardiovascular events.
Corticosteroids
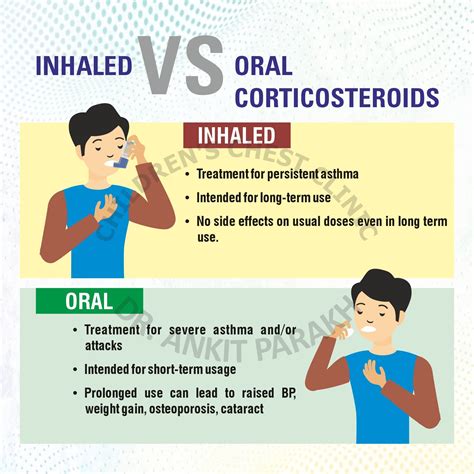
Corticosteroids are potent anti-inflammatory medications that are often used to treat inflammatory pain. They work by suppressing the production of pro-inflammatory cytokines and reducing the activity of immune cells. Commonly used corticosteroids include:
- Prednisone
- Methylprednisolone
- Dexamethasone
- Hydrocortisone
Corticosteroids can be administered orally, intravenously, or via injection into the affected joint or tissue. They are effective in reducing inflammation and pain but can have significant side effects, such as weight gain, mood changes, and increased risk of infections.
Biologics
Biologics are a class of medications that target specific molecules involved in the inflammatory response. Examples of biologics used to treat inflammatory pain include: * TNF-alpha inhibitors (e.g., etanercept, adalimumab) * IL-1β inhibitors (e.g., anakinra) * IL-6 inhibitors (e.g., tocilizumab)Biologics are often used to treat conditions such as rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. They can be effective in reducing inflammation and pain but may increase the risk of infections and other side effects.
Disease-Modifying Antirheumatic Drugs (DMARDs)
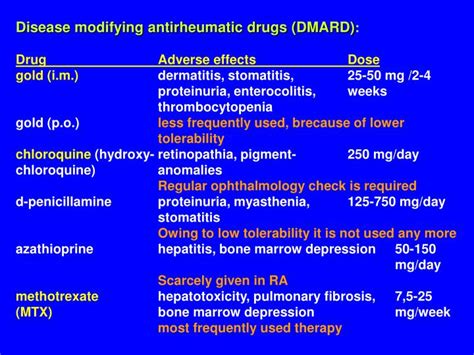
DMARDs are a class of medications that are used to treat inflammatory conditions such as rheumatoid arthritis. They work by modifying the underlying disease process, reducing inflammation, and slowing disease progression. Examples of DMARDs include:
- Methotrexate
- Sulfasalazine
- Hydroxychloroquine
- Leflunomide
DMARDs can be effective in reducing inflammation and pain but may have significant side effects, such as gastrointestinal toxicity, liver damage, and increased risk of infections.
Other Medications
Other medications that may be used to treat inflammatory pain include: * Muscle relaxants (e.g., cyclobenzaprine) * Anticonvulsants (e.g., gabapentin) * Opioids (e.g., morphine, codeine)These medications can be effective in reducing pain but may have significant side effects, such as addiction, constipation, and respiratory depression.
Conclusion and Future Directions

In conclusion, the management of inflammatory pain involves a comprehensive approach, including lifestyle modifications, physical therapy, and pharmacological interventions. NSAIDs, corticosteroids, biologics, and DMARDs are commonly used to treat inflammatory pain, each with its own mechanism of action and potential side effects. As research continues to uncover the underlying mechanisms of inflammatory pain, new and innovative treatments are being developed, offering hope for improved pain management and quality of life.
We invite you to share your thoughts and experiences with inflammatory pain management. Have you found any of these medications or treatments effective in reducing your pain? What challenges have you faced in managing your condition? Your comments and feedback are valuable in helping us better understand the complexities of inflammatory pain and developing more effective treatment strategies.
What is the best medication for inflammatory pain?
+The best medication for inflammatory pain depends on the underlying condition, disease severity, and individual patient factors. NSAIDs, corticosteroids, biologics, and DMARDs are commonly used to treat inflammatory pain, each with its own mechanism of action and potential side effects.
How can I reduce inflammation and pain without medication?
+Lifestyle modifications, such as maintaining a healthy weight, exercising regularly, and following an anti-inflammatory diet, can help reduce inflammation and pain. Additionally, stress management techniques, such as meditation and yoga, can also be beneficial in reducing pain and improving overall well-being.
What are the potential side effects of biologics?
+Biologics can increase the risk of infections, such as tuberculosis and fungal infections. They can also cause allergic reactions, infusion reactions, and injection site reactions. Additionally, biologics may increase the risk of certain types of cancer, such as lymphoma.
