Intro
Discover how cholestasis in pregnancy impacts health, from itching to liver function, and learn about intrahepatic cholestasis of pregnancy symptoms, diagnosis, and management to ensure a safe pregnancy and childbirth experience.
Cholestasis is a liver condition that can significantly impact pregnancy, affecting both the mother and the fetus. It is essential to understand the effects of cholestasis on pregnancy to ensure the best possible outcomes for both. Cholestasis of pregnancy, also known as obstetric cholestasis, is a condition characterized by a reduction in the flow of bile from the liver, leading to a buildup of bile acids in the bloodstream. This condition can cause severe itching, jaundice, and other complications, making it crucial for pregnant women to be aware of its implications.
Pregnancy is a complex and delicate process, and any underlying medical conditions can have significant effects on both the mother and the developing fetus. Cholestasis, in particular, can have far-reaching consequences, from mild discomfort to severe complications. As such, it is vital to recognize the signs and symptoms of cholestasis and seek medical attention promptly to prevent any adverse outcomes. By understanding the effects of cholestasis on pregnancy, expectant mothers can take proactive steps to manage their condition and ensure a healthy pregnancy.
The relationship between cholestasis and pregnancy is multifaceted, and several factors contribute to the development of this condition during pregnancy. Hormonal changes, genetic predisposition, and environmental factors can all play a role in the onset of cholestasis. As the condition progresses, it can lead to a range of complications, including premature birth, fetal distress, and even stillbirth. Therefore, it is crucial to monitor the condition closely and take proactive measures to mitigate its effects.
Introduction to Cholestasis and Pregnancy

Causes and Risk Factors of Cholestasis
The exact causes of cholestasis are not fully understood, but several factors can increase the risk of developing the condition during pregnancy. These include a history of cholestasis in previous pregnancies, a family history of the condition, and certain genetic mutations. Additionally, women who are carrying twins or multiple fetuses are at a higher risk of developing cholestasis. Understanding the causes and risk factors of cholestasis is crucial in identifying women who may be at risk and providing them with appropriate care and management.Effects of Cholestasis on Pregnancy
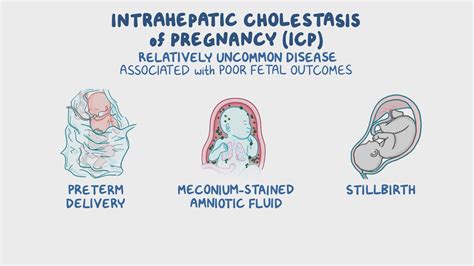
- Premature birth: Cholestasis can increase the risk of premature birth, which can lead to a range of complications for the baby.
- Fetal distress: The buildup of bile acids in the bloodstream can cause fetal distress, which can lead to stillbirth or other complications.
- Low birth weight: Babies born to mothers with cholestasis may have a lower birth weight, which can increase the risk of health problems.
- Increased risk of meconium aspiration syndrome: Cholestasis can increase the risk of meconium aspiration syndrome, a condition in which the baby inhales meconium during delivery.
Managing Cholestasis During Pregnancy
Managing cholestasis during pregnancy requires a comprehensive approach that involves medication, lifestyle changes, and close monitoring. Some of the key strategies for managing cholestasis include:- Medication: Ursodeoxycholic acid (UDCA) is a medication that can help reduce the levels of bile acids in the bloodstream.
- Lifestyle changes: Avoiding foods that trigger itching, staying hydrated, and getting regular exercise can help manage symptoms.
- Close monitoring: Regular check-ups with a healthcare provider can help monitor the condition and prevent complications.
Treatment Options for Cholestasis
- Ursodeoxycholic acid (UDCA): This medication can help reduce the levels of bile acids in the bloodstream.
- S-adenosylmethionine (SAMe): This supplement can help improve liver function and reduce symptoms.
- Vitamin K: This vitamin can help prevent bleeding complications.
Preventing Complications of Cholestasis
Preventing complications of cholestasis requires close monitoring and proactive management. Some of the key strategies for preventing complications include:- Regular check-ups: Regular check-ups with a healthcare provider can help monitor the condition and prevent complications.
- Fetal monitoring: Regular fetal monitoring can help detect any signs of fetal distress.
- Induction of labor: In some cases, induction of labor may be necessary to prevent complications.
Living with Cholestasis During Pregnancy
- Staying hydrated: Drinking plenty of water can help reduce symptoms.
- Avoiding triggers: Avoiding foods that trigger itching and other symptoms can help manage the condition.
- Getting regular exercise: Regular exercise can help improve liver function and reduce symptoms.
Coping with the Emotional Impact of Cholestasis
Coping with the emotional impact of cholestasis during pregnancy can be challenging, but there are several strategies that can help. Some of the key strategies include:- Seeking support: Seeking support from family, friends, and healthcare providers can help manage the emotional impact of the condition.
- Practicing stress-reducing techniques: Practicing stress-reducing techniques, such as meditation and deep breathing, can help manage stress and anxiety.
- Staying informed: Staying informed about the condition and its management can help reduce anxiety and improve outcomes.
Conclusion and Next Steps
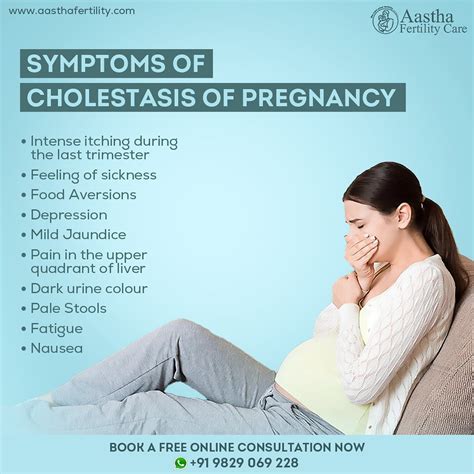
What are the symptoms of cholestasis during pregnancy?
+The symptoms of cholestasis during pregnancy include intense itching, jaundice, dark urine, and pale stools. In some cases, women may also experience fatigue, loss of appetite, and nausea.
How is cholestasis diagnosed during pregnancy?
+Cholestasis is diagnosed during pregnancy through a combination of physical examination, medical history, and laboratory tests. Laboratory tests may include liver function tests, bile acid tests, and ultrasound scans.
What are the treatment options for cholestasis during pregnancy?
+Treatment options for cholestasis during pregnancy include medication, such as ursodeoxycholic acid (UDCA), and lifestyle changes, such as avoiding foods that trigger itching and staying hydrated. In some cases, induction of labor may be necessary to prevent complications.
Can cholestasis during pregnancy increase the risk of complications?
+Yes, cholestasis during pregnancy can increase the risk of complications, including premature birth, fetal distress, and stillbirth. It is essential to work closely with healthcare providers to manage the condition and prevent complications.
How can women with cholestasis during pregnancy manage their symptoms and improve their quality of life?
+Women with cholestasis during pregnancy can manage their symptoms and improve their quality of life by staying hydrated, avoiding foods that trigger itching, getting regular exercise, and practicing stress-reducing techniques. Seeking support from family, friends, and healthcare providers can also help manage the emotional impact of the condition.
We hope this article has provided you with a comprehensive understanding of cholestasis and its effects on pregnancy. If you have any further questions or concerns, please do not hesitate to reach out to your healthcare provider. Additionally, we encourage you to share this article with others who may be affected by cholestasis during pregnancy, and to join the conversation on social media using the hashtag #cholestasisawareness. By working together, we can raise awareness and improve outcomes for women with cholestasis during pregnancy.
