Intro
Discover 5 uses of Clindamycin, a broad-spectrum antibiotic, for treating bacterial infections, acne, skin infections, and more, with its antimicrobial properties and effectiveness against anaerobic bacteria.
The importance of antibiotics in modern medicine cannot be overstated. Among the numerous antibiotics available, Clindamycin stands out due to its broad spectrum of activity and effectiveness against various bacterial infections. Clindamycin is a lincosamide antibiotic that has been widely used for decades to treat infections caused by Gram-positive and certain Gram-negative bacteria. Its versatility and efficacy have made it a staple in the treatment of numerous conditions, ranging from skin and soft tissue infections to more severe diseases like pneumonia and septicemia.
Clindamycin's mechanism of action involves inhibiting protein synthesis in bacteria, which is crucial for their growth and replication. This inhibition is achieved by binding to the 50S subunit of the bacterial ribosome, thereby preventing the formation of peptide bonds and ultimately leading to the death of the bacterial cells. This unique mechanism of action, combined with its ability to penetrate into various tissues and fluids, makes Clindamycin an effective choice for treating infections in different parts of the body.
The application of Clindamycin extends across various medical specialties, including dermatology, orthopedics, and infectious diseases. Its use is not limited to treating established infections but also as a prophylactic measure to prevent infections in certain surgical procedures. The broad-spectrum activity of Clindamycin, its availability in both oral and parenteral forms, and its generally favorable safety profile have contributed to its widespread adoption in clinical practice. However, like all antibiotics, the use of Clindamycin must be judicious and guided by principles of antimicrobial stewardship to minimize the risk of resistance and adverse effects.
Introduction to Clindamycin
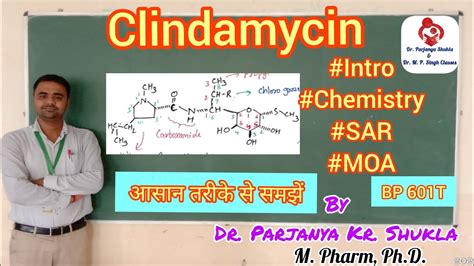
Clindamycin is derived from lincomycin, another antibiotic, and was developed to improve upon the latter's spectrum of activity and pharmacokinetic properties. Since its introduction into clinical practice, Clindamycin has been used to treat a wide range of bacterial infections. Its effectiveness against anaerobic bacteria, in particular, has made it a valuable option in the treatment of infections where these organisms are commonly involved, such as in abdominal, pelvic, and skin infections.
Uses of Clindamycin

The uses of Clindamycin can be broadly categorized based on the type of infection being treated. Some of the primary uses include:
- Skin and Soft Tissue Infections: Clindamycin is effective against infections such as cellulitis, abscesses, and wound infections caused by bacteria like Staphylococcus aureus and Streptococcus pyogenes.
- Respiratory Tract Infections: It is used to treat pneumonia and other lower respiratory tract infections, particularly those caused by anaerobic bacteria.
- Bone and Joint Infections: Clindamycin is used in the treatment of osteomyelitis (bone infection) and septic arthritis (joint infection), often in conjunction with other antibiotics.
- Gynecological Infections: It is effective in treating pelvic inflammatory disease (PID), which involves infection of the female reproductive organs.
- Dental Infections: Clindamycin can be used to treat dental infections, including abscesses and infections following dental procedures.
Benefits of Clindamycin
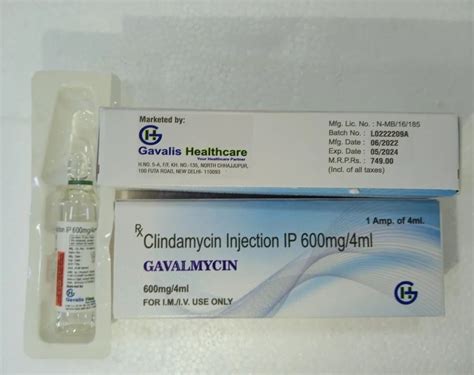
The benefits of using Clindamycin include its broad-spectrum activity, the availability of both oral and intravenous formulations, and its ability to penetrate into various tissues and fluids, including bone. This makes it an effective option for treating infections in different parts of the body. Additionally, Clindamycin has been shown to be effective against certain bacteria that are resistant to other antibiotics, making it a valuable option in cases where resistance is a concern.Administration and Dosage

The administration and dosage of Clindamycin depend on the type and severity of the infection, as well as the patient's age, weight, and renal function. Clindamycin can be administered orally in the form of capsules or liquid, or intravenously in a hospital setting. The dosage ranges from 150 to 450 mg orally every six to eight hours for adults, with adjustments made for pediatric patients and those with impaired renal function.
Side Effects and Contraindications
While Clindamycin is generally well-tolerated, it can cause side effects, including gastrointestinal disturbances like diarrhea, nausea, and vomiting. More serious side effects include pseudomembranous colitis, which is a potentially life-threatening condition caused by the overgrowth of Clostridioides difficile (C. diff) in the colon. Clindamycin is contraindicated in patients with a history of hypersensitivity to the drug or lincomycin, and its use should be approached with caution in patients with a history of gastrointestinal disease.Resistance and Stewardship
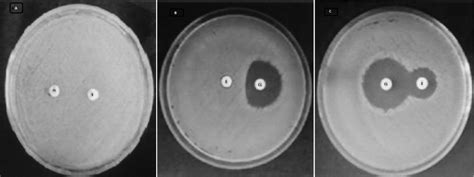
The emergence of antibiotic resistance is a significant concern with the use of any antibiotic, including Clindamycin. Resistance can develop through various mechanisms, including the production of enzymes that inactivate the antibiotic and alterations in the target site of the antibiotic. To mitigate the risk of resistance, it is essential to use Clindamycin judiciously, following principles of antimicrobial stewardship. This includes using the antibiotic only when necessary, selecting the appropriate dosage and duration of therapy, and monitoring for signs of resistance.
Future Perspectives
Given the ongoing challenge of antibiotic resistance, research into new antibiotics and alternative therapies is crucial. For Clindamycin, future perspectives may include the development of new formulations or combinations with other antibiotics to enhance its efficacy and reduce the risk of resistance. Additionally, efforts to improve antimicrobial stewardship and reduce unnecessary antibiotic use will be essential in preserving the effectiveness of Clindamycin and other antibiotics for future generations.Conclusion and Recommendations

In conclusion, Clindamycin is a valuable antibiotic with a broad spectrum of activity against various bacterial infections. Its effectiveness, combined with its availability in different formulations, makes it a versatile option in clinical practice. However, its use must be guided by principles of antimicrobial stewardship to minimize the risk of resistance and adverse effects. Healthcare professionals should be aware of the benefits and limitations of Clindamycin, as well as the importance of judicious antibiotic use, to ensure that this valuable antibiotic remains effective for the treatment of bacterial infections.
Final Thoughts
As we move forward in the era of increasing antibiotic resistance, it is crucial to approach the use of antibiotics like Clindamycin with caution and respect. By doing so, we can ensure that these valuable drugs continue to be effective in treating bacterial infections, thereby saving countless lives and improving patient outcomes. The responsible use of Clindamycin and other antibiotics is a collective effort that requires the participation of healthcare professionals, patients, and policymakers to promote antimicrobial stewardship and reduce the threat of antibiotic resistance.
Engagement and Action
We invite readers to share their thoughts and experiences with Clindamycin and antibiotic use in general. Your insights can help raise awareness about the importance of responsible antibiotic use and the need for continued research into new antibiotics and alternative therapies. By working together, we can ensure that antibiotics like Clindamycin remain effective for generations to come. Please feel free to comment below, share this article with others, or take action by supporting initiatives that promote antimicrobial stewardship and combat antibiotic resistance.
What is Clindamycin used for?
+Clindamycin is used to treat various bacterial infections, including skin and soft tissue infections, respiratory tract infections, bone and joint infections, gynecological infections, and dental infections.
How does Clindamycin work?
+Clindamycin works by inhibiting protein synthesis in bacteria, which is essential for their growth and replication. It binds to the 50S subunit of the bacterial ribosome, preventing the formation of peptide bonds and ultimately leading to the death of the bacterial cells.
What are the side effects of Clindamycin?
+Common side effects of Clindamycin include gastrointestinal disturbances like diarrhea, nausea, and vomiting. More serious side effects can include pseudomembranous colitis, a potentially life-threatening condition caused by the overgrowth of Clostridioides difficile (C. diff) in the colon.
Why is it important to use Clindamycin judiciously?
+Using Clindamycin judiciously is important to minimize the risk of antibiotic resistance and adverse effects. This includes using the antibiotic only when necessary, selecting the appropriate dosage and duration of therapy, and monitoring for signs of resistance.
What can be done to promote antimicrobial stewardship?
+Promoting antimicrobial stewardship involves a collective effort from healthcare professionals, patients, and policymakers. This can include initiatives such as educating patients about the proper use of antibiotics, implementing antibiotic stewardship programs in healthcare settings, and supporting research into new antibiotics and alternative therapies.
