Intro
Diagnose gluten enteropathy with a blood test, detecting celiac disease and non-celiac gluten sensitivity through antibody screenings, intestinal damage assessment, and genetic testing for accurate diagnosis and treatment.
The importance of accurate diagnosis in managing gluten-related disorders cannot be overstated. Among these conditions, gluten enteropathy, also known as celiac disease, is a chronic autoimmune disorder that causes the immune system to react to gluten, leading to damage in the small intestine. This condition can lead to malabsorption of nutrients, causing a variety of symptoms that can range from mild to severe. The diagnosis of gluten enteropathy is multifaceted, involving clinical evaluation, serological tests, and intestinal biopsy. Among these diagnostic tools, blood tests play a crucial role in identifying individuals with gluten enteropathy.
Gluten enteropathy affects a significant portion of the population worldwide, though its prevalence can vary greatly among different regions and populations. The condition is often underdiagnosed or misdiagnosed, which can lead to prolonged suffering and increased risk of complications such as malnutrition, osteoporosis, and even certain types of cancer. The advent of sensitive and specific blood tests has significantly improved the ability to diagnose gluten enteropathy, enabling healthcare providers to initiate appropriate management strategies early on. Understanding the mechanisms, benefits, and limitations of these blood tests is essential for both healthcare professionals and individuals suspected of having the condition.
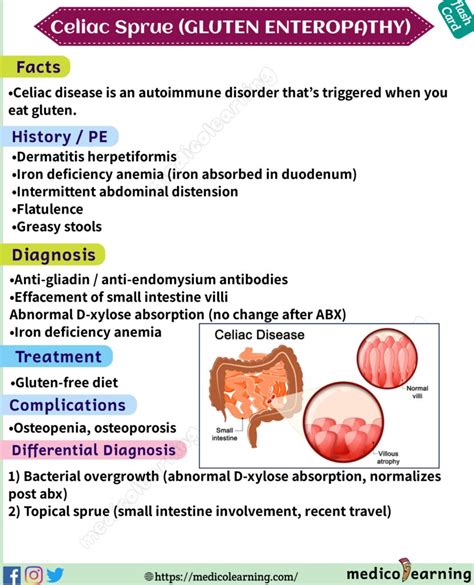
The pathophysiology of gluten enteropathy involves an immune response to gluten, a protein found in wheat, barley, and rye, which leads to inflammation and damage to the villi of the small intestine. This damage impairs the ability of the intestine to absorb nutrients, resulting in a wide range of clinical manifestations. The diagnosis of gluten enteropathy is based on a combination of clinical presentation, serological tests, and histological examination of the small intestine. Blood tests are a critical component of this diagnostic process, offering a non-invasive means to detect the presence of certain antibodies associated with the condition.
Understanding Gluten Enteropathy Blood Tests
Gluten enteropathy blood tests are designed to detect the presence of specific autoantibodies that are produced in response to gluten. These autoantibodies include endomysial antibodies (EMA), tissue transglutaminase antibodies (tTGA), and deamidated gliadin peptide antibodies (DGP). The presence of these antibodies in the blood is a strong indicator of an immune response to gluten and, by extension, gluten enteropathy. Each of these tests has its own sensitivity and specificity, and they are often used in combination to enhance diagnostic accuracy.
Types of Blood Tests
The choice of blood test can depend on various factors, including the patient's age, clinical presentation, and the availability of testing facilities. For instance, the tTGA test is widely used and has high sensitivity and specificity for gluten enteropathy, especially in individuals with European ancestry. On the other hand, DGP tests can be useful in diagnosing the condition in individuals who are already on a gluten-free diet, as these antibodies can remain positive for a longer period after gluten exposure.Interpreting Blood Test Results
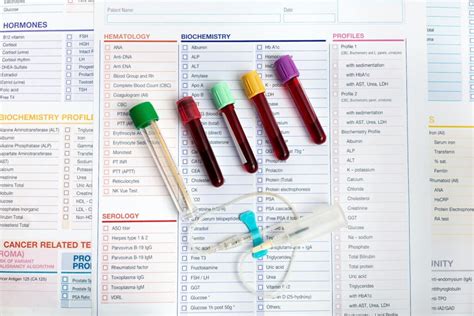
Interpreting the results of gluten enteropathy blood tests requires careful consideration of several factors, including the clinical context, the presence of symptoms, and the results of other diagnostic tests such as intestinal biopsy. A positive result on any of the serological tests suggests the presence of an immune response to gluten but does not definitively diagnose gluten enteropathy. Conversely, a negative result does not entirely rule out the condition, especially if the individual has been on a gluten-free diet for some time before testing.
Clinical Context and Symptom Evaluation
The clinical context and symptom evaluation play a crucial role in the interpretation of blood test results. Symptoms such as diarrhea, abdominal pain, fatigue, and weight loss are common in gluten enteropathy but can also be present in other conditions. Therefore, the presence of these symptoms, combined with positive serological tests, strengthens the diagnosis of gluten enteropathy.The Role of Intestinal Biopsy
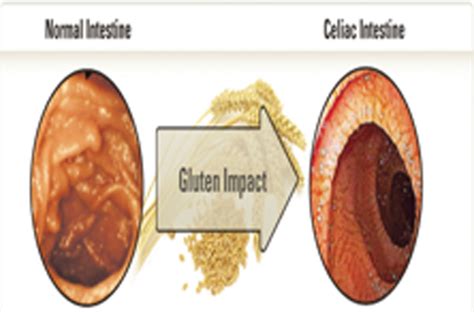
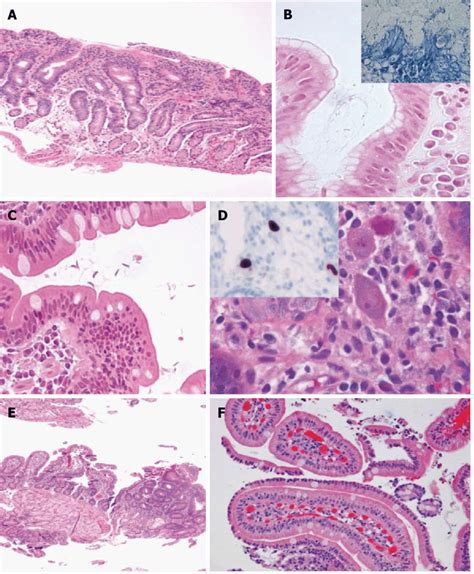
While blood tests are invaluable in the diagnostic process, intestinal biopsy remains the gold standard for confirming the diagnosis of gluten enteropathy. This procedure involves the collection of tissue samples from the small intestine, which are then examined for signs of damage and inflammation. The presence of villous atrophy, crypt hyperplasia, and increased intraepithelial lymphocytes are characteristic findings in gluten enteropathy.
Benefits and Limitations of Intestinal Biopsy
Intestinal biopsy offers a direct visualization of the intestinal mucosa, providing definitive evidence of the extent of damage caused by gluten. However, the procedure is invasive, requiring endoscopy, and may not be suitable for all patients, especially children and those with certain medical conditions. Furthermore, the interpretation of biopsy results can be subjective and may vary between different pathologists.Management and Treatment of Gluten Enteropathy
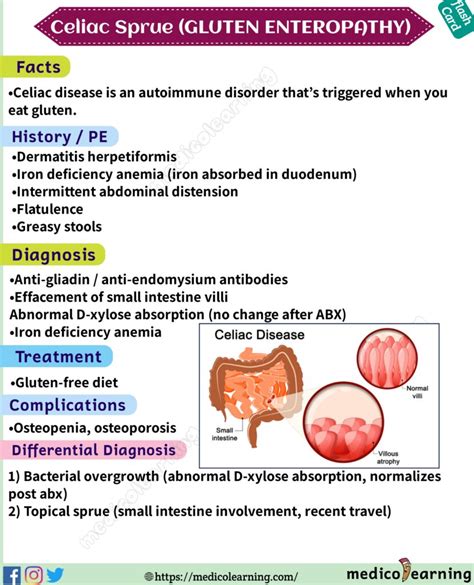
The management of gluten enteropathy primarily involves the adoption of a strict gluten-free diet. This dietary change can lead to the healing of the intestinal mucosa, improvement in symptoms, and reduction in the risk of complications. Adherence to the diet can be challenging and requires significant lifestyle adjustments, including careful reading of food labels, avoidance of cross-contamination with gluten, and seeking out gluten-free alternatives.
Challenges in Gluten-Free Diet Adherence
Maintaining a gluten-free diet can be challenging due to the ubiquity of gluten in many food products, the risk of cross-contamination, and the higher cost of gluten-free foods. Additionally, individuals with gluten enteropathy may need to ensure they are getting adequate nutrients, as the condition can lead to deficiencies in iron, calcium, and vitamin B12, among others.Future Directions in Gluten Enteropathy Diagnosis and Treatment
Research into gluten enteropathy is ongoing, with efforts focused on improving diagnostic tests, understanding the genetic and environmental factors that contribute to the condition, and developing new treatments. Potential future directions include the development of non-invasive diagnostic tests that can detect the condition without the need for intestinal biopsy, and the exploration of therapeutic strategies that can reduce or eliminate the need for a gluten-free diet.
Emerging Therapies and Technologies
Emerging therapies for gluten enteropathy include the use of enzymes that can break down gluten, making it less toxic to individuals with the condition. Additionally, technologies that can detect gluten in food and environments with high accuracy are being developed, which could significantly improve the quality of life for individuals with gluten enteropathy.What are the common symptoms of gluten enteropathy?
+Common symptoms include diarrhea, abdominal pain, fatigue, weight loss, and malabsorption of nutrients.
How is gluten enteropathy diagnosed?
+Diagnosis involves a combination of clinical evaluation, serological tests (blood tests), and intestinal biopsy.
What is the treatment for gluten enteropathy?
+The primary treatment is a strict gluten-free diet, which can lead to the healing of the intestinal mucosa and improvement in symptoms.
In conclusion, the diagnosis and management of gluten enteropathy are complex processes that require a comprehensive approach, including clinical evaluation, serological testing, and intestinal biopsy. Blood tests play a crucial role in the diagnostic process, offering a non-invasive means to detect the presence of autoantibodies associated with the condition. As research continues to uncover the intricacies of gluten enteropathy, it is essential for individuals suspected of having the condition to consult with healthcare professionals to initiate appropriate diagnostic and therapeutic strategies. We invite readers to share their experiences with gluten enteropathy, ask questions, and explore the resources available for managing this condition effectively.
