Intro
Discover the role of HCG hormone levels in pregnancy, including normal ranges, testing, and fluctuations, to understand its impact on fetal development and maternal health during early pregnancy stages and trimesters.
The human chorionic gonadotropin (hCG) hormone plays a vital role in pregnancy, serving as a crucial indicator of the health and progression of the pregnancy. hCG is produced by the placenta shortly after implantation of the fertilized egg into the uterine lining. This hormone helps maintain the corpus luteum, which is essential for producing progesterone, a hormone necessary for fetal development. Understanding hCG hormone levels in pregnancy is essential for monitoring the pregnancy's progress and identifying any potential issues.
During the early stages of pregnancy, hCG levels can provide valuable insights into the pregnancy's viability and health. In a normal pregnancy, hCG levels typically follow a predictable pattern, doubling approximately every 48 hours during the first trimester. This rapid increase in hCG levels is essential for supporting the growth and development of the embryo. As the pregnancy progresses, hCG levels continue to rise, peaking around the 10th week of gestation. After this peak, hCG levels gradually decline, stabilizing at a lower level for the remainder of the pregnancy.
The significance of monitoring hCG hormone levels in pregnancy cannot be overstated. Abnormal hCG levels can be an indicator of potential complications, such as ectopic pregnancy, miscarriage, or chromosomal abnormalities. For example, low hCG levels may suggest a non-viable pregnancy or an ectopic pregnancy, while extremely high hCG levels may be associated with conditions like molar pregnancy or Down syndrome. Therefore, healthcare providers closely monitor hCG levels to ensure the pregnancy is progressing as expected and to identify any potential issues early on.
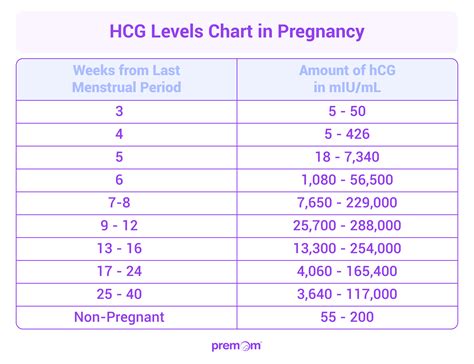
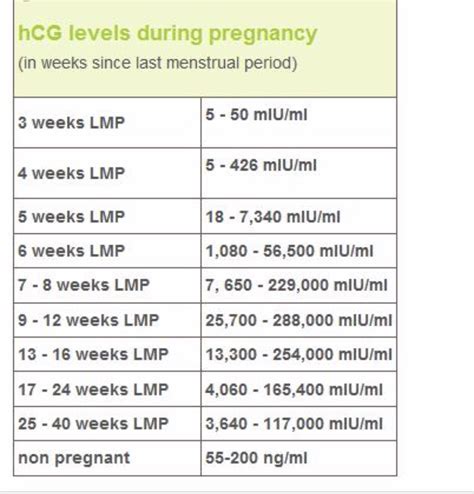
hCG Levels Throughout Pregnancy
hCG levels vary significantly throughout pregnancy, with the most rapid increases occurring during the first trimester. Here's a breakdown of typical hCG levels during different stages of pregnancy:
- 1-2 weeks: 5-50 mIU/mL
- 2-3 weeks: 50-500 mIU/mL
- 3-4 weeks: 100-5,000 mIU/mL
- 4-5 weeks: 1,000-20,000 mIU/mL
- 5-6 weeks: 5,000-50,000 mIU/mL
- 6-7 weeks: 10,000-100,000 mIU/mL
- 7-10 weeks: 20,000-200,000 mIU/mL
- 10-12 weeks: 50,000-200,000 mIU/mL Keep in mind that these are general ranges, and hCG levels can vary significantly from one woman to another.
Factors Influencing hCG Levels
Several factors can influence hCG levels, including: * Multiple pregnancy: Women carrying twins or other multiples tend to have higher hCG levels. * Fetal age: hCG levels are typically higher in pregnancies with older fetuses. * Maternal weight: Obese women may have lower hCG levels due to the increased distance between the embryo and the maternal bloodstream. * Time of day: hCG levels can fluctuate throughout the day, with peak levels usually occurring in the morning. * Laboratory variability: Different laboratories may use varying testing methods, which can result in slightly different hCG level readings.Abnormal hCG Levels
Abnormal hCG levels can be an indicator of potential complications during pregnancy. Some common causes of abnormal hCG levels include:
- Ectopic pregnancy: Low or slowly rising hCG levels may suggest an ectopic pregnancy, where the fertilized egg implants outside the uterus.
- Miscarriage: Low or declining hCG levels can indicate a non-viable pregnancy or an impending miscarriage.
- Molar pregnancy: Extremely high hCG levels may be associated with a molar pregnancy, a rare condition where the placenta develops abnormally.
- Down syndrome: High hCG levels may be linked to an increased risk of Down syndrome or other chromosomal abnormalities.
hCG Level Monitoring
Regular monitoring of hCG levels is essential for ensuring the pregnancy is progressing as expected. Healthcare providers typically perform hCG level tests: * During the first trimester to confirm pregnancy and monitor fetal development * To diagnose and monitor ectopic pregnancy or miscarriage * To screen for chromosomal abnormalities, such as Down syndrome * To monitor fetal growth and development throughout the pregnancyhCG Levels and Pregnancy Complications
Abnormal hCG levels can be an indicator of potential pregnancy complications. Some common complications associated with abnormal hCG levels include:
- Preeclampsia: High hCG levels may be linked to an increased risk of preeclampsia, a condition characterized by high blood pressure and damage to organs such as the kidneys and liver.
- Gestational diabetes: Abnormal hCG levels may be associated with an increased risk of gestational diabetes, a condition characterized by high blood sugar levels during pregnancy.
- Fetal growth restriction: Low hCG levels may indicate fetal growth restriction, a condition where the fetus does not grow at a normal rate.
Pregnancy Loss and hCG Levels
Pregnancy loss, including miscarriage and stillbirth, can be a devastating experience for expectant mothers. Abnormal hCG levels can be an indicator of pregnancy loss, and regular monitoring can help healthcare providers identify potential issues early on. Some common signs of pregnancy loss include: * Vaginal bleeding or spotting * Severe abdominal pain or cramping * Low or declining hCG levels * Fetal demise or absence of fetal heartbeathCG Levels and Multiple Pregnancy
Women carrying twins or other multiples tend to have higher hCG levels due to the increased number of placentas producing the hormone. However, hCG levels can vary significantly between multiple pregnancies, and healthcare providers must carefully monitor hCG levels to ensure the pregnancy is progressing as expected. Some common characteristics of hCG levels in multiple pregnancy include:
- Higher peak hCG levels: Women carrying multiples tend to have higher peak hCG levels, often exceeding 200,000 mIU/mL.
- Faster hCG doubling time: hCG levels tend to double more rapidly in multiple pregnancies, often every 24-36 hours.
- Increased risk of complications: Multiple pregnancies are associated with an increased risk of complications, including preeclampsia, gestational diabetes, and fetal growth restriction.
hCG Levels and Fetal Development
hCG levels play a crucial role in supporting fetal development, particularly during the first trimester. The hormone helps maintain the corpus luteum, which produces progesterone, essential for fetal growth and development. Abnormal hCG levels can be an indicator of potential issues with fetal development, including: * Fetal growth restriction: Low hCG levels may indicate fetal growth restriction, a condition where the fetus does not grow at a normal rate. * Congenital abnormalities: Abnormal hCG levels may be associated with an increased risk of congenital abnormalities, such as heart defects or cleft palate.Monitoring hCG Levels at Home

While healthcare providers typically monitor hCG levels through blood tests, women can also use home pregnancy tests to detect the presence of hCG in their urine. These tests are often less sensitive than blood tests but can provide a general indication of hCG levels. Some common characteristics of home pregnancy tests include:
- Sensitivity: Home pregnancy tests typically have a sensitivity of 20-50 mIU/mL, meaning they can detect hCG levels above this threshold.
- Accuracy: Home pregnancy tests are generally accurate when used correctly, but false positives or false negatives can occur.
- Timing: Home pregnancy tests can be used as early as 6-8 days post-ovulation, but accuracy improves as hCG levels increase.
Interpreting hCG Levels
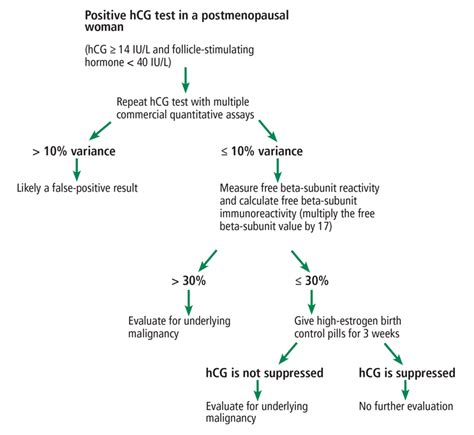
Interpreting hCG levels requires careful consideration of various factors, including the stage of pregnancy, maternal weight, and laboratory variability. Healthcare providers use hCG levels to: * Confirm pregnancy: hCG levels are used to confirm pregnancy and monitor fetal development. * Diagnose ectopic pregnancy: Abnormal hCG levels can indicate an ectopic pregnancy, and healthcare providers may use hCG levels to diagnose and monitor this condition. * Screen for chromosomal abnormalities: hCG levels are used in conjunction with other screening tests to identify potential chromosomal abnormalities, such as Down syndrome.hCG Levels and Pregnancy Outcome
Abnormal hCG levels can be an indicator of potential complications during pregnancy, and regular monitoring is essential for ensuring the best possible outcome. Some common factors that influence pregnancy outcome include:
- Fetal growth and development: Abnormal hCG levels can affect fetal growth and development, increasing the risk of complications.
- Placental function: The placenta plays a critical role in supporting fetal development, and abnormal hCG levels can indicate issues with placental function.
- Maternal health: Maternal health, including conditions like preeclampsia and gestational diabetes, can influence pregnancy outcome and be reflected in abnormal hCG levels.
Pregnancy Complications and hCG Levels
Pregnancy complications, such as preeclampsia and gestational diabetes, can be associated with abnormal hCG levels. Healthcare providers must carefully monitor hCG levels to identify potential issues early on and provide appropriate management. Some common complications that can affect hCG levels include: * Preeclampsia: High hCG levels may be linked to an increased risk of preeclampsia, a condition characterized by high blood pressure and damage to organs such as the kidneys and liver. * Gestational diabetes: Abnormal hCG levels may be associated with an increased risk of gestational diabetes, a condition characterized by high blood sugar levels during pregnancy.Conclusion and Next Steps

In conclusion, hCG hormone levels play a vital role in pregnancy, serving as a crucial indicator of the health and progression of the pregnancy. Understanding hCG levels is essential for monitoring fetal development, identifying potential complications, and ensuring the best possible outcome. By staying informed and working closely with healthcare providers, expectant mothers can navigate the complexities of pregnancy and make informed decisions about their care.
If you have any questions or concerns about hCG hormone levels in pregnancy, we encourage you to share your thoughts and experiences in the comments below. Additionally, feel free to share this article with friends and family who may be interested in learning more about this topic.
What is the normal range for hCG levels in pregnancy?
+hCG levels vary significantly throughout pregnancy, but typical ranges include 5-50 mIU/mL at 1-2 weeks, 50-500 mIU/mL at 2-3 weeks, and 100-5,000 mIU/mL at 3-4 weeks.
What do abnormal hCG levels indicate?
+Abnormal hCG levels can indicate potential complications, such as ectopic pregnancy, miscarriage, or chromosomal abnormalities. Low hCG levels may suggest a non-viable pregnancy or an ectopic pregnancy, while extremely high hCG levels may be associated with conditions like molar pregnancy or Down syndrome.
How often should hCG levels be monitored during pregnancy?
+hCG levels are typically monitored during the first trimester to confirm pregnancy and monitor fetal development. Healthcare providers may also monitor hCG levels to diagnose and monitor ectopic pregnancy or miscarriage, screen for chromosomal abnormalities, and monitor fetal growth and development throughout the pregnancy.
Can home pregnancy tests detect hCG levels?
+Yes, home pregnancy tests can detect the presence of hCG in urine, but they are often less sensitive than blood tests. Home pregnancy tests typically have a sensitivity of 20-50 mIU/mL, meaning they can detect hCG levels above this threshold.
What factors can influence hCG levels?
+Several factors can influence hCG levels, including multiple pregnancy, fetal age, maternal weight, time of day, and laboratory variability. Healthcare providers must carefully consider these factors when interpreting hCG levels.
