Intro
Discover Heparin Induced Thrombocytopenia (HIT) causes, symptoms, and treatment. Learn about low platelet count, blood clotting, and anticoagulant risks, understanding HIT syndrome and its management.
Heparin-induced thrombocytopenia, commonly referred to as HIT, is a serious medical condition that occurs in some individuals who receive heparin, a blood thinner used to prevent and treat blood clots. Despite its purpose of preventing clotting, heparin can paradoxically trigger the formation of blood clots in certain people, leading to a potentially life-threatening situation. Understanding the complexities of HIT is crucial for both healthcare professionals and patients, as early recognition and appropriate management can significantly improve outcomes.
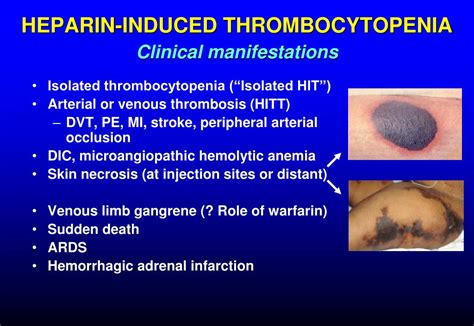
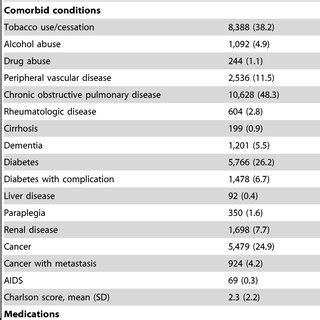
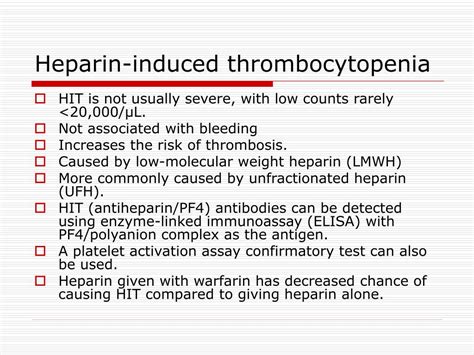
The importance of recognizing HIT lies in its potential to cause significant morbidity and mortality. It is estimated that HIT affects approximately 0.2% to 5% of patients who receive heparin, depending on the type of heparin used, the dose, and the duration of treatment. The condition can lead to the formation of blood clots in both arteries and veins, increasing the risk of heart attacks, strokes, and other thrombotic complications. Furthermore, HIT can also result in thrombocytopenia, a condition characterized by low platelet counts, which can further increase the risk of bleeding and clotting complications.
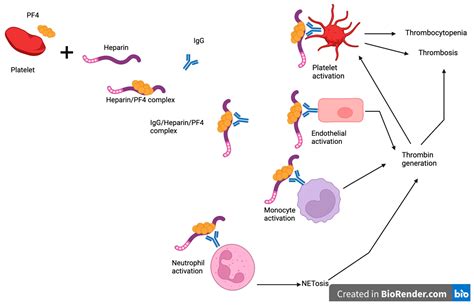
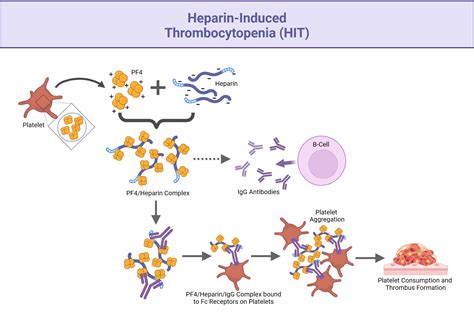
The pathophysiology of HIT involves an immune-mediated response to heparin. When heparin binds to platelet factor 4 (PF4), a protein found on platelets, it can trigger the formation of antibodies. These antibodies can then activate platelets, leading to the release of pro-coagulant microparticles and the formation of blood clots. The activation of platelets also leads to their consumption, resulting in thrombocytopenia. Understanding this complex process is essential for the diagnosis and management of HIT, as it highlights the importance of early recognition and the need for alternative anticoagulation strategies.
Introduction to Heparin-Induced Thrombocytopenia
Clinical Presentation of Heparin-Induced Thrombocytopenia
Diagnostic Criteria for Heparin-Induced Thrombocytopenia
The diagnosis of HIT is based on a combination of clinical and laboratory criteria. The 4T score is a widely used scoring system that evaluates the likelihood of HIT based on four criteria: thrombocytopenia, timing of thrombocytopenia, thrombosis, and absence of other causes of thrombocytopenia. A score of 4 or more indicates a high probability of HIT, while a score of 0-3 indicates a low probability. Laboratory tests, such as the PF4 enzyme-linked immunosorbent assay (ELISA) and the serotonin release assay (SRA), can also be used to confirm the diagnosis.Management of Heparin-Induced Thrombocytopenia
Prevention of Heparin-Induced Thrombocytopenia
Prevention of HIT is crucial, particularly in patients who are at high risk of developing the condition. This can be achieved by using alternative anticoagulants, such as low molecular weight heparin (LMWH) or fondaparinux, which have a lower risk of inducing HIT. Regular monitoring of platelet counts is also essential, particularly in patients who are receiving heparin therapy. In some cases, patients may require platelet count monitoring every other day, particularly if they have a history of HIT or are at high risk of developing the condition.Complications of Heparin-Induced Thrombocytopenia
Treatment of Thrombotic Complications
The treatment of thrombotic complications in HIT involves the use of anticoagulants that do not cross-react with heparin-induced antibodies. Direct thrombin inhibitors, such as argatroban and bivalirudin, can be used to treat thrombotic complications, particularly in patients who have a high risk of bleeding. Fondaparinux, a factor Xa inhibitor, can also be used in some cases. The goal of treatment is to prevent further thrombotic complications and to manage any existing thrombosis.Future Directions in Heparin-Induced Thrombocytopenia
Emerging Therapies for Heparin-Induced Thrombocytopenia
Emerging therapies for HIT include the use of novel anticoagulants, such as factor XI inhibitors, and the development of new diagnostic tests. Gene therapy may also offer a potential treatment option for HIT, particularly in patients who have a genetic predisposition to developing the condition. Additionally, research is being conducted to develop new treatments that can reverse the effects of heparin-induced antibodies, allowing for the safe use of heparin in patients who are at high risk of developing HIT.What is heparin-induced thrombocytopenia?
+Heparin-induced thrombocytopenia is a serious medical condition that occurs in some individuals who receive heparin, a blood thinner used to prevent and treat blood clots.
What are the symptoms of heparin-induced thrombocytopenia?
+The symptoms of HIT can vary, but they typically involve a decrease in platelet count, often accompanied by thrombotic complications, such as chest pain, shortness of breath, or neurological deficits.
How is heparin-induced thrombocytopenia diagnosed?
+The diagnosis of HIT is based on a combination of clinical and laboratory criteria, including the 4T score and laboratory tests, such as the PF4 ELISA and the SRA.
What is the treatment for heparin-induced thrombocytopenia?
+The treatment of HIT involves the immediate discontinuation of heparin therapy and the initiation of alternative anticoagulation strategies, such as direct thrombin inhibitors or factor Xa inhibitors.
Can heparin-induced thrombocytopenia be prevented?
+Prevention of HIT is crucial, particularly in patients who are at high risk of developing the condition. This can be achieved by using alternative anticoagulants, such as LMWH or fondaparinux, and regular monitoring of platelet counts.
In conclusion, heparin-induced thrombocytopenia is a complex and potentially life-threatening condition that requires prompt recognition and management. By understanding the pathophysiology, clinical presentation, and treatment options for HIT, healthcare professionals can provide optimal care for patients who are at risk of developing this condition. As research continues to evolve, new diagnostic tests and treatment options may become available, offering improved outcomes for patients with HIT. We invite you to share your thoughts and experiences with heparin-induced thrombocytopenia, and to ask any questions you may have about this complex condition.
