Intro
Understand the International Normalized Ratio (INR), a blood test measuring clotting time, and its significance in monitoring anticoagulation therapy, bleeding risks, and warfarin treatment, ensuring optimal patient care and thrombosis prevention.
The International Normalized Ratio, commonly referred to as INR, is a crucial component in the management and treatment of patients who are on anticoagulant therapy, particularly those taking warfarin. Understanding INR is essential not only for healthcare professionals but also for patients who need to monitor their condition closely to ensure their safety and the effectiveness of their treatment. The importance of INR lies in its ability to standardize the results of the prothrombin time (PT) test, which measures how long it takes for blood to clot. This standardization is vital because different laboratories may use different reagents for the PT test, which can lead to variations in results. By standardizing these results through the INR, healthcare providers can make informed decisions about patient care, regardless of where the blood tests were conducted.
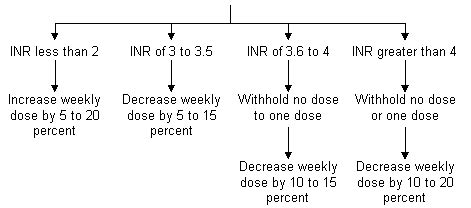
The need for a standardized measurement like INR arose from the complexities of managing anticoagulation therapy. Patients on warfarin, for example, require regular monitoring to ensure that their blood is within the therapeutic range - not too prone to clotting, which could lead to strokes or other thrombotic events, but also not too thin, which could increase the risk of bleeding. The therapeutic range for most indications is typically between an INR of 2.0 and 3.0, though this can vary depending on the specific condition being treated. For instance, patients with mechanical heart valves may require a higher INR to prevent valve thrombosis, while those with atrial fibrillation may be managed at a lower INR to balance the risk of stroke against the risk of bleeding.
Understanding how INR works is also crucial for patient safety. An INR that is too high indicates that the blood is too thin and the patient is at an increased risk of bleeding. Conversely, an INR that is too low suggests that the blood is not thin enough, potentially leading to the formation of dangerous blood clots. Patients and their healthcare providers must work together to maintain the INR within the target range, adjusting doses of anticoagulant medications as necessary. This collaborative approach to managing INR not only improves patient outcomes but also empowers patients to take an active role in their healthcare, learning to recognize the signs of both bleeding and clotting and knowing when to seek medical attention.
Introduction to INR
The concept of INR is fundamentally about standardizing the measurement of blood clotting. The prothrombin time (PT) test, which INR is derived from, measures the time it takes for plasma to clot after addition of tissue factor. However, the PT can vary significantly between different laboratories due to differences in the sensitivity of the thromboplastin reagents used in the test. The INR calculation adjusts for this variability by using the International Sensitivity Index (ISI) of the thromboplastin reagent. This means that regardless of where a patient's blood is tested, the INR result will be comparable, allowing for more consistent and reliable monitoring of anticoagulation therapy.
How INR Works
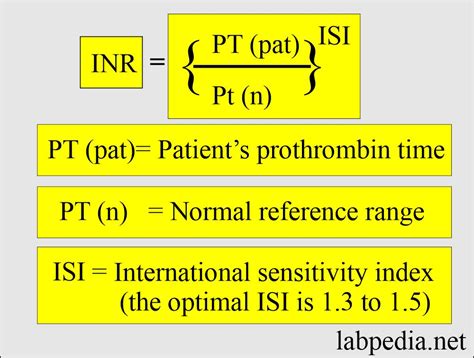
The calculation of INR involves the patient's PT result and the ISI of the thromboplastin used, along with the mean normal prothrombin time (MNPT) for the laboratory. The formula for INR is INR = (PT / MNPT)^ISI. This formula ensures that the results are standardized and can be compared across different laboratories. Understanding how INR is calculated can help patients appreciate the complexity and importance of their anticoagulation therapy. It also underscores the need for regular monitoring and adjustments to their treatment plan to maintain the INR within the therapeutic range.
Benefits of INR
The benefits of using INR in the management of anticoagulation therapy are numerous. It allows for the standardization of results, making it easier to compare patient data across different healthcare settings. This standardization also facilitates the adjustment of anticoagulant doses, ensuring that patients receive the most effective and safest level of anticoagulation. Moreover, the use of INR has been shown to reduce the risk of both thrombotic and bleeding complications in patients on warfarin, ultimately improving patient outcomes and quality of life.Monitoring INR

Monitoring INR is a critical aspect of anticoagulation therapy. Patients on warfarin typically need to have their INR checked regularly, with the frequency depending on their stability and the specific clinical situation. For patients who are newly started on warfarin or have had recent dose changes, more frequent monitoring may be necessary to ensure that their INR is within the therapeutic range. This monitoring can be done through venipuncture at a laboratory or, increasingly, through point-of-care devices that allow patients to check their INR at home. Home monitoring can improve the convenience and frequency of INR checks, potentially leading to better control of anticoagulation and reduced risks of complications.
Importance of Patient Education
Patient education plays a vital role in the successful management of anticoagulation therapy and INR monitoring. Patients need to understand the importance of maintaining their INR within the therapeutic range, how to recognize signs of bleeding or clotting, and when to seek medical attention. They should also be aware of factors that can affect their INR, such as changes in diet (especially vitamin K intake), other medications, and alcohol consumption. By empowering patients with knowledge, healthcare providers can enhance patient safety, improve adherence to treatment plans, and ultimately achieve better outcomes.Challenges and Considerations

Despite the benefits of INR monitoring, there are challenges and considerations that healthcare providers and patients must be aware of. One of the main challenges is ensuring that patients maintain their INR within the therapeutic range, which can be affected by various factors including diet, other medications, and patient compliance. Additionally, the use of warfarin, the most common anticoagulant for which INR is monitored, has its own set of challenges, including a narrow therapeutic window and the potential for drug interactions. Newer anticoagulants, such as direct oral anticoagulants (DOACs), offer alternatives but do not require INR monitoring, which can simplify management for some patients but may also limit the ability to adjust therapy based on laboratory results.
Future Directions
The management of anticoagulation therapy and INR monitoring is an evolving field. Research continues into new anticoagulants and monitoring technologies that could simplify therapy and improve patient outcomes. Point-of-care INR devices, for example, are becoming more prevalent, allowing for more frequent monitoring and potentially better control of anticoagulation. Furthermore, studies are exploring the use of genetic information to predict warfarin dose requirements, which could lead to more personalized and effective anticoagulation therapy. As these advancements emerge, healthcare providers and patients must stay informed to ensure that they are benefiting from the latest developments in anticoagulation management.Conclusion and Next Steps

In conclusion, understanding INR is crucial for the effective management of anticoagulation therapy. By grasping the principles of INR, including how it is calculated, its benefits, and the challenges associated with its monitoring, patients and healthcare providers can work together to optimize anticoagulation therapy. This collaborative approach, combined with ongoing advancements in anticoagulation management, holds the promise of improving patient outcomes and reducing the risks associated with blood clots and bleeding.
Call to Action

We invite readers to share their experiences with INR monitoring and anticoagulation therapy. Your stories and insights can help others understand the importance of this aspect of healthcare and how it impacts daily life. Additionally, we encourage healthcare professionals to continue their education on the latest developments in anticoagulation management, including new technologies and therapies that can improve patient care. By working together and staying informed, we can advance the field of anticoagulation therapy and improve outcomes for patients worldwide.
Final Thoughts
As we look to the future of anticoagulation therapy and INR monitoring, it is clear that there are many opportunities for improvement and innovation. From the development of new anticoagulants to advancements in point-of-care testing, the potential to enhance patient care and outcomes is significant. We hope that this article has provided a comprehensive overview of INR and its role in anticoagulation therapy, and we look forward to continuing the conversation on this critical topic.
What is INR and why is it important?
+INR, or International Normalized Ratio, is a test used to measure blood clotting and is crucial for patients on anticoagulant therapy, particularly those taking warfarin. It helps standardize the results of the prothrombin time (PT) test, allowing for better management of anticoagulation and reducing the risk of bleeding or clotting complications.
How often should INR be monitored?
+The frequency of INR monitoring depends on the individual patient's stability and specific clinical situation. Patients who are newly started on warfarin or have had recent dose changes may require more frequent monitoring, while those who are stable may need less frequent checks.
What factors can affect INR results?
+Several factors can affect INR results, including changes in diet (especially vitamin K intake), other medications, alcohol consumption, and patient compliance with their anticoagulation regimen. It is essential for patients to be aware of these factors to maintain their INR within the therapeutic range.
