Intro
Discover how low blood CO2 levels impact health, causing respiratory issues, fatigue, and anxiety, through 5 key effects on respiratory alkalosis, breathing, and overall wellbeing, highlighting CO2 importance.
The importance of maintaining proper blood CO2 levels cannot be overstated. Carbon dioxide, often viewed as a waste product, plays a crucial role in various bodily functions, including the regulation of blood pH, the transport of oxygen to tissues, and the maintenance of blood vessel diameter. Low blood CO2, also known as hypocapnia, can have far-reaching consequences on overall health and well-being. This condition can arise from various factors, including hyperventilation, certain medical conditions, and high-altitude environments. Understanding the effects of low blood CO2 on health is essential for preventing and managing related disorders.
The human body operates within a narrow range of blood CO2 levels, typically between 35 and 45 mmHg. Deviations from this range can disrupt normal physiological processes, leading to a variety of symptoms and health issues. Hypocapnia, in particular, can cause respiratory alkalosis, a condition characterized by an increase in blood pH due to the decreased levels of carbonic acid. This imbalance can affect multiple systems in the body, from the nervous system to the cardiovascular system. The consequences of low blood CO2 can be subtle at first but may escalate into severe health problems if left unaddressed.
Low blood CO2 levels can result from deliberate actions, such as deep or rapid breathing, often practiced in meditation, yoga, or as a response to stress. While these practices can offer benefits when performed correctly and in moderation, excessive or improper breathing techniques can lead to hypocapnia. Additionally, certain medical conditions, such as asthma, chronic obstructive pulmonary disease (COPD), and pneumonia, can cause low blood CO2 levels due to altered breathing patterns or respiratory function. High-altitude environments, where the air pressure is lower, can also lead to hypocapnia due to the body's attempt to adapt to the decreased oxygen availability by increasing breathing rate.
Physiological Effects of Low Blood CO2
Respiratory Alkalosis
Respiratory alkalosis is a direct consequence of low blood CO2 levels. When carbon dioxide is decreased, the blood becomes more alkaline, disrupting the body's acid-base balance. This condition can lead to a range of symptoms, including muscle cramps, spasms, and tetany, due to the altered ionized calcium levels in the blood. The nervous system is also affected, with potential symptoms ranging from anxiety and panic attacks to seizures in severe cases. Understanding and managing respiratory alkalosis is crucial for mitigating the effects of low blood CO2 on overall health.Clinical Presentation and Diagnosis

Treatment and Management
Treatment and management of low blood CO2 focus on addressing the underlying cause and alleviating symptoms. For cases induced by hyperventilation, breathing exercises that promote slower, deeper breathing can help restore normal CO2 levels. In instances where medical conditions are the cause, managing the underlying disease is crucial. This may involve medications to control symptoms, respiratory therapy to improve lung function, and lifestyle modifications to reduce stress and promote healthy breathing habits. In severe cases, hospitalization may be necessary to monitor and manage complications.Prevention Strategies

Lifestyle Modifications
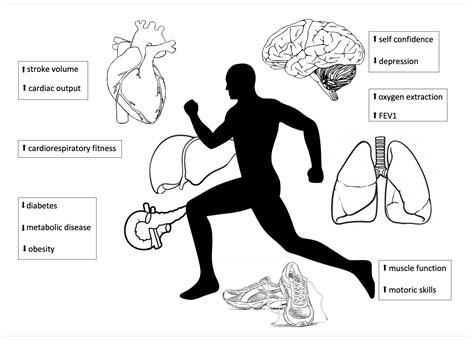
Lifestyle modifications play a significant role in preventing and managing low blood CO2 levels. This includes avoiding excessive alcohol consumption, quitting smoking, and maintaining a healthy weight to reduce the risk of developing conditions that could lead to hypocapnia. Engaging in regular physical activity can improve respiratory function and overall health, while a diet rich in fruits, vegetables, and whole grains can provide essential nutrients for optimal bodily functions. Additionally, practicing relaxation techniques, such as deep breathing exercises (when done correctly), progressive muscle relaxation, and mindfulness, can help manage stress and prevent hyperventilation.Complications and Long-Term Effects
Quality of Life and Cognitive Function
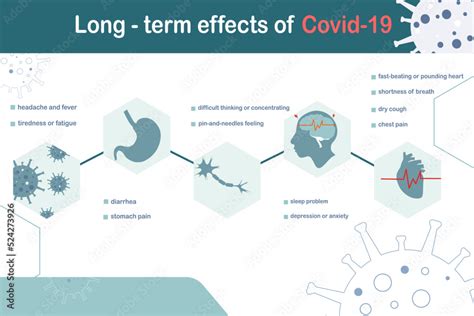
The impact of low blood CO2 on quality of life and cognitive function should not be underestimated. Persistent symptoms such as dizziness, anxiety, and confusion can significantly impair daily activities and social interactions. Cognitive function may also be affected, with potential decreases in concentration, memory, and decision-making abilities. Addressing low blood CO2 levels through appropriate treatment and lifestyle modifications is crucial for mitigating these effects and improving overall quality of life.Future Research Directions

Novel Therapeutic Approaches
The development of novel therapeutic approaches for managing low blood CO2 levels is an area of ongoing research. This includes the exploration of pharmacological interventions that can help stabilize blood CO2 levels, as well as innovative respiratory therapies designed to improve gas exchange and reduce symptoms. Furthermore, the integration of complementary therapies, such as mindfulness and relaxation techniques, into standard treatment protocols may offer additional benefits in terms of symptom management and quality of life.What are the primary causes of low blood CO2 levels?
+Primary causes include hyperventilation, certain medical conditions like asthma and COPD, and high-altitude environments.
How is low blood CO2 diagnosed?
+Diagnosis is typically made through arterial blood gas analysis, which measures blood CO2 levels directly.
What are the long-term effects of untreated low blood CO2 levels?
+Untreated low blood CO2 can lead to chronic respiratory issues, cardiovascular complications, and persistent neurological symptoms.
In conclusion, the importance of maintaining adequate blood CO2 levels for overall health cannot be overstated. Understanding the causes, symptoms, and management strategies for low blood CO2 is essential for healthcare providers and individuals at risk. By adopting preventive measures, recognizing early symptoms, and seeking appropriate medical care, individuals can mitigate the effects of low blood CO2 and maintain optimal health. We invite readers to share their experiences, ask questions, and engage in discussions about the critical role of blood CO2 in health and disease, fostering a community that values knowledge sharing and mutual support.
