Intro
Discover 5 ways to diagnose Lyme disease, including symptom analysis, blood tests, and physical exams, to accurately identify this tick-borne illness and prevent misdiagnosis, ensuring timely treatment and recovery from its debilitating effects.
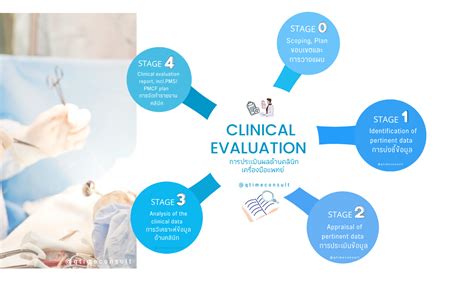
Lyme disease, a bacterial infection caused by Borrelia burgdorferi, is primarily transmitted to humans through the bite of an infected blacklegged tick. The disease can lead to a range of symptoms, from mild to severe, including fever, headache, fatigue, and a distinctive skin rash known as erythema migrans. Given its complexity and the potential for long-term health consequences if left untreated, accurate and timely diagnosis of Lyme disease is crucial. The diagnosis of Lyme disease can be challenging due to its nonspecific symptoms, which can mimic other conditions, and the limitations of diagnostic tests. Here, we delve into the various methods used for diagnosing Lyme disease, highlighting the importance of a comprehensive approach that combines clinical evaluation, laboratory testing, and sometimes, empirical treatment based on clinical judgment.
The early diagnosis of Lyme disease is critical for effective treatment and prevention of long-term complications. Healthcare providers typically start by conducting a thorough medical history and physical examination to look for signs and symptoms consistent with Lyme disease, such as the characteristic "bull's-eye" rash, fever, and joint pain. However, not all patients develop this rash, and some may present with nonspecific symptoms that could be attributed to other illnesses, making the clinical diagnosis challenging.
Laboratory Tests for Lyme Disease

Clinical Evaluation and Empirical Treatment
Understanding False Negatives and False Positives
It's essential to understand that no diagnostic test is perfect. False negatives can occur if the test is performed too early in the course of the disease, before the body has produced antibodies against B. burgdorferi. False positives can result from cross-reactivity with other infections or from the presence of residual antibodies from a past infection. Healthcare providers must interpret test results in the context of the patient's clinical presentation and sometimes may need to repeat tests or use additional diagnostic tools to confirm the diagnosis.Diagnostic Challenges and Controversies

Post-Treatment Lyme Disease Syndrome (PTLDS)
PTLDS is a condition characterized by lingering symptoms of fatigue, muscle and joint pain, and cognitive difficulties that last for more than six months after completion of antibiotic therapy for Lyme disease. The exact cause of PTLDS is not well understood, but it is thought to result from residual damage to tissues and the immune system caused by the infection, rather than ongoing infection. Treatment for PTLDS is primarily supportive, focusing on managing symptoms and improving quality of life, as there is currently no evidence that prolonged antibiotic treatment is beneficial.Future Directions in Lyme Disease Diagnosis

Public Awareness and Prevention
Public awareness and education about Lyme disease are critical for its prevention and early diagnosis. Individuals living in or visiting areas where Lyme disease is common should take preventive measures, such as using insect repellents, wearing protective clothing, and conducting regular tick checks after spending time outdoors. Prompt removal of attached ticks can prevent the transmission of the bacteria, as the tick typically needs to be attached for at least 36 to 48 hours to transmit the infection.Treatment and Management of Lyme Disease

Long-Term Prognosis and Quality of Life
For most patients, prompt and appropriate treatment of Lyme disease leads to a full recovery. However, some individuals may experience persistent symptoms, highlighting the importance of follow-up care and sometimes, additional treatment or supportive therapies to manage symptoms and improve quality of life. Ongoing research aims to better understand the factors that contribute to long-term outcomes and to develop more effective treatments for patients with persistent symptoms.Conclusion and Future Outlook

We invite readers to share their experiences or ask questions about Lyme disease diagnosis and treatment in the comments below. This exchange can foster a community of support and provide valuable insights for those navigating the challenges of Lyme disease. Additionally, sharing this article with others can help spread awareness about the importance of early diagnosis and the need for continued research into this complex condition.
What are the early symptoms of Lyme disease?
+The early symptoms of Lyme disease can include a distinctive skin rash (erythema migrans), fever, headache, fatigue, and joint pain, though not all patients develop the rash.
How is Lyme disease diagnosed?
+Lyme disease is diagnosed through a combination of clinical evaluation (medical history and physical examination), laboratory tests (such as ELISA and Western blot), and sometimes, empirical treatment based on clinical judgment.
What is the treatment for Lyme disease?
+The treatment for Lyme disease typically involves a course of antibiotics, with the specific regimen depending on the stage and severity of the disease. Early-stage Lyme disease can often be treated with oral antibiotics.
Can Lyme disease be prevented?
+While there is no guaranteed way to prevent Lyme disease, individuals can reduce their risk by using insect repellents, wearing protective clothing, conducting regular tick checks, and promptly removing attached ticks.
What is post-treatment Lyme disease syndrome (PTLDS)?
+PTLDS refers to a condition where patients experience lingering symptoms of fatigue, muscle and joint pain, and cognitive difficulties for more than six months after completing antibiotic treatment for Lyme disease.
