Intro
The importance of understanding metronidazole adverse effects cannot be overstated, as this medication is widely used to treat various infections caused by bacteria and protozoa. Metronidazole, also known by its brand name Flagyl, is a nitroimidazole antibiotic that has been a cornerstone in the treatment of infections such as trichomoniasis, amoebiasis, and giardiasis, among others. Despite its effectiveness, metronidazole can cause a range of side effects, from mild to severe, which necessitates a thorough understanding of its adverse effects to ensure safe and effective use.
Metronidazole's mechanism of action involves the interference with the DNA of microbial cells, ultimately leading to cell death. This targeted action is beneficial in eliminating the causative agents of infections. However, the same mechanism can also affect human cells, particularly when used in high doses or for prolonged periods, leading to various adverse effects. The severity and likelihood of these effects can vary depending on the dose, duration of treatment, and individual patient factors such as age, liver function, and the presence of other health conditions.
The management and prevention of metronidazole adverse effects are crucial aspects of patient care. Healthcare providers must weigh the benefits of metronidazole treatment against the potential risks, considering alternative treatments when necessary. Patients, too, play a significant role by being aware of the possible side effects and reporting any concerns to their healthcare provider promptly. This collaborative approach helps in minimizing the risk of adverse effects and ensuring the safe use of metronidazole.
Introduction to Metronidazole

Metronidazole is a synthetic antibiotic that belongs to the class of nitroimidazoles. It is effective against a wide range of organisms, including both aerobic and anaerobic bacteria, as well as protozoa. The drug works by entering the cells of the microorganisms and damaging their DNA, which prevents them from reproducing and ultimately leads to their death. This unique mechanism of action makes metronidazole particularly useful in treating infections caused by organisms that are resistant to other types of antibiotics.
Pharmacokinetics and Pharmacodynamics
The pharmacokinetics of metronidazole involves its absorption, distribution, metabolism, and excretion. After oral administration, metronidazole is well absorbed from the gastrointestinal tract, with peak plasma concentrations reached within 1-3 hours. The drug is widely distributed throughout the body and crosses the blood-brain barrier. Metronidazole is metabolized in the liver, and its metabolites are excreted in the urine. Understanding the pharmacokinetics and pharmacodynamics of metronidazole is essential for optimizing its therapeutic effects and minimizing its adverse effects.Common Adverse Effects of Metronidazole

The common adverse effects of metronidazole can be categorized into gastrointestinal, neurological, dermatological, and hematological effects, among others. Gastrointestinal side effects include nausea, vomiting, diarrhea, and abdominal pain. These effects are usually mild and transient but can be severe enough to warrant discontinuation of the drug in some cases. Neurological effects, such as headache, dizziness, and metallic taste, are also common. Dermatological reactions, including rash and itching, can occur, although they are less frequent.
Gastrointestinal Side Effects
Gastrointestinal side effects are among the most common adverse effects of metronidazole. These can range from mild nausea and vomiting to more severe diarrhea and abdominal pain. In some cases, patients may experience a metallic taste, which can be distressing. To minimize these effects, metronidazole is often taken with food, although this may not entirely prevent gastrointestinal side effects.Severe Adverse Effects of Metronidazole
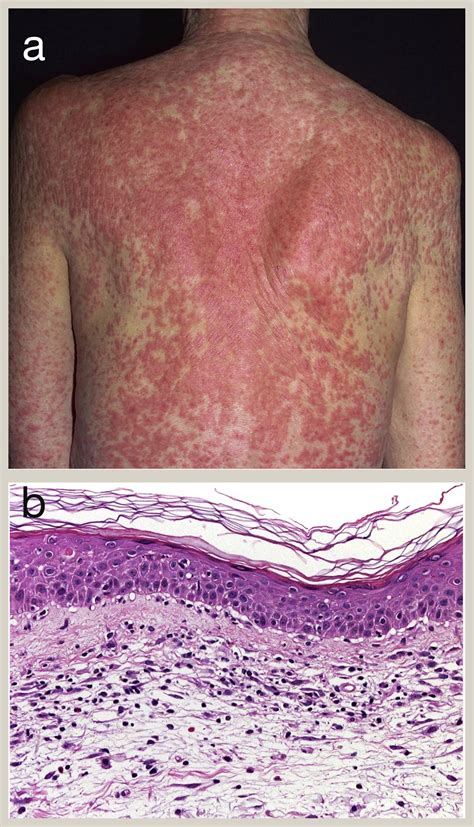
While less common, severe adverse effects of metronidazole can occur and may require immediate medical attention. These include severe allergic reactions, such as anaphylaxis, which can be life-threatening. Other severe effects include seizures, peripheral neuropathy, and blood dyscrasias, such as leukopenia and thrombocytopenia. The risk of these severe effects is higher with prolonged use or in patients with pre-existing conditions that may predispose them to these adverse effects.
Neurotoxicity and Peripheral Neuropathy
Neurotoxicity, including peripheral neuropathy, is a recognized severe adverse effect of metronidazole. This condition can manifest as numbness, tingling, or pain in the hands and feet and can be irreversible in some cases. The risk of neurotoxicity is dose-dependent and is more likely to occur with high doses or prolonged treatment. Patients should be closely monitored for signs of neurotoxicity, and metronidazole should be discontinued if symptoms occur.Metronidazole Use in Special Populations

The use of metronidazole in special populations, such as pregnant women, children, and patients with liver or kidney disease, requires careful consideration. In pregnancy, metronidazole is generally avoided during the first trimester due to the potential risk of teratogenic effects. However, it may be used in the second and third trimesters if the benefits outweigh the risks. In children, the dosage of metronidazole must be adjusted according to their weight to minimize the risk of adverse effects.
Pregnancy and Lactation
The safety of metronidazole during pregnancy and lactation is a concern due to its potential effects on the fetus and newborn. While metronidazole crosses the placenta, its use during the second and third trimesters is considered safe when necessary. However, during lactation, metronidazole is excreted in breast milk, and its use should be avoided or breastfeeding should be discontinued during treatment.Interactions with Other Medications

Metronidazole can interact with various medications, either enhancing or reducing their effects. For example, the concurrent use of metronidazole with warfarin can increase the risk of bleeding due to the inhibition of warfarin metabolism. Similarly, metronidazole can interact with phenytoin, leading to increased phenytoin levels and potential toxicity. Understanding these interactions is crucial for preventing adverse effects and ensuring the safe use of metronidazole.
Alcohol and Metronidazole Interaction
The interaction between alcohol and metronidazole is significant, as alcohol can potentiate the adverse effects of metronidazole, particularly gastrointestinal and neurological effects. Patients are advised to avoid alcohol consumption during and for at least 24 hours after metronidazole treatment to minimize the risk of these interactions.Management and Prevention of Adverse Effects

The management and prevention of metronidazole adverse effects involve a combination of strategies, including dose adjustment, monitoring for side effects, and patient education. Healthcare providers should closely monitor patients for signs of adverse effects, especially during the initial stages of treatment. Patients should be educated on the potential side effects, the importance of adherence to the prescribed regimen, and the need to report any concerns promptly.
Patient Education and Adherence
Patient education plays a vital role in the safe use of metronidazole. Patients should be informed about the potential adverse effects, the importance of completing the full treatment course, and the need to avoid alcohol during treatment. Adherence to the prescribed regimen is crucial for maximizing the therapeutic effects of metronidazole while minimizing its adverse effects.Conclusion and Future Directions
In conclusion, metronidazole is a valuable antibiotic for the treatment of various infections, but its use is associated with a range of adverse effects. Understanding these effects, from common gastrointestinal side effects to severe neurotoxicity, is essential for the safe and effective use of metronidazole. Future directions in the management of metronidazole adverse effects may include the development of new formulations or analogs with improved safety profiles and the optimization of treatment regimens to minimize the risk of adverse effects.
Final Thoughts
As research continues to evolve, it is crucial for healthcare providers and patients to stay informed about the latest developments in the use of metronidazole and its adverse effects. By working together, we can ensure the safe and effective use of this important antibiotic, minimizing its risks while maximizing its benefits.What are the most common adverse effects of metronidazole?
+The most common adverse effects of metronidazole include gastrointestinal side effects such as nausea, vomiting, diarrhea, and abdominal pain, as well as neurological effects like headache and dizziness.
Can metronidazole cause severe adverse effects?
+Yes, metronidazole can cause severe adverse effects, including severe allergic reactions, seizures, peripheral neuropathy, and blood dyscrasias. These effects are less common but can be serious and require immediate medical attention.
How can the risk of metronidazole adverse effects be minimized?
+The risk of metronidazole adverse effects can be minimized by using the lowest effective dose for the shortest duration necessary, monitoring patients for signs of adverse effects, and educating patients on the potential risks and the importance of adherence to the prescribed regimen.
We invite readers to share their experiences or ask questions about metronidazole adverse effects in the comments section below. Your input can help others understand the importance of being aware of these effects and how to manage them effectively. Additionally, feel free to share this article with anyone who might benefit from this information, and let's work together to promote safe and informed use of metronidazole.
