Intro
Discover 5 ways pre-eclampsia affects pregnancy, including high blood pressure, eclampsia risks, and placental abruption, to ensure a healthy birth and prevent complications like gestational hypertension and preeclampsia symptoms.
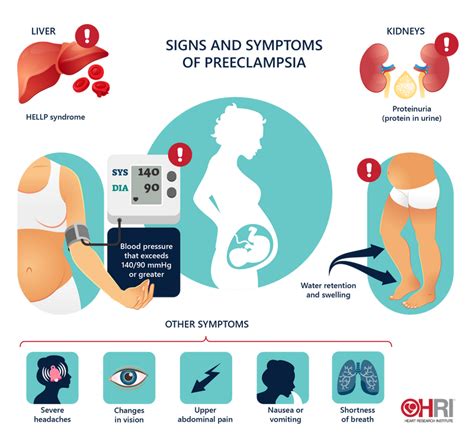
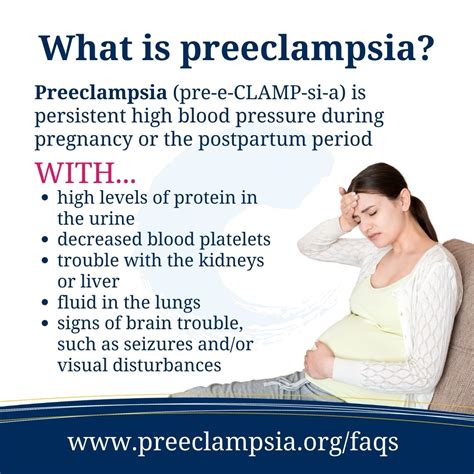
Pre-eclampsia is a pregnancy complication characterized by high blood pressure and often accompanied by significant amounts of protein in the urine. This condition can lead to serious complications for both the mother and the baby if left untreated. It is crucial for pregnant women to understand the risks and symptoms associated with pre-eclampsia to ensure timely medical intervention. The importance of recognizing pre-eclampsia cannot be overstated, as it is a leading cause of maternal and fetal morbidity and mortality worldwide. Understanding the condition, its symptoms, and how it can be managed is essential for all expectant mothers.
Pre-eclampsia affects a significant number of pregnancies, and its impact can be severe. The condition is diagnosed after 20 weeks of gestation and can lead to premature birth, low birth weight, and in severe cases, eclampsia, which involves seizures. Given the potential risks, it is vital to monitor blood pressure regularly during prenatal check-ups and to report any symptoms that could indicate pre-eclampsia, such as severe headaches, vision changes, and abdominal pain. Early detection and appropriate management are key to preventing complications and ensuring the best possible outcomes for both mother and baby.
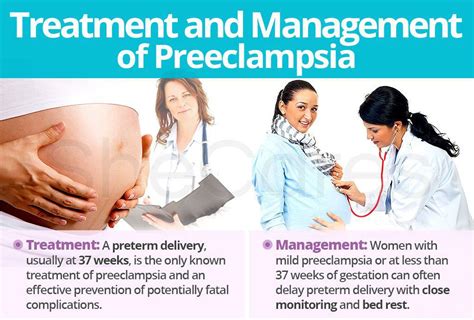
The management of pre-eclampsia involves careful monitoring of the mother's and fetus's condition, with the goal of balancing the need to prevent the condition from worsening against the desire to allow the pregnancy to progress as far as safely possible. This can involve hospitalization for close monitoring, bed rest, and in some cases, medication to lower blood pressure or prevent seizures. In severe cases, the only cure for pre-eclampsia is delivery, which may be induced or performed via cesarean section, depending on the gestational age and the health of the mother and baby. Understanding these aspects of pre-eclampsia management can empower women to take an active role in their pregnancy care.
Understanding Pre-Eclampsia

Risk Factors for Pre-Eclampsia
Several risk factors have been identified for pre-eclampsia, including a history of high blood pressure, kidney disease, or a previous pregnancy complicated by pre-eclampsia. Additionally, women carrying multiple fetuses, those with a history of certain medical conditions like diabetes or autoimmune disorders, and those who are obese or have a family history of pre-eclampsia are at a higher risk. Recognizing these risk factors can help healthcare providers to closely monitor at-risk pregnancies and intervene early if signs of pre-eclampsia develop.Diagnosing Pre-Eclampsia
Managing Pre-Eclampsia
The management of pre-eclampsia depends on the severity of the condition and the gestational age of the fetus. For women with mild pre-eclampsia at or near term, delivery is often the recommended course of action, as it is the only cure for the condition. For those diagnosed before term, careful monitoring is crucial to balance the risks of preterm birth against the risks of allowing the condition to worsen. This may involve bed rest, close monitoring of blood pressure and fetal well-being, and in some cases, corticosteroids to promote fetal lung maturity in anticipation of preterm delivery.Treatments for Pre-Eclampsia
Preventing Pre-Eclampsia
While there is no guaranteed way to prevent pre-eclampsia, certain measures can reduce the risk. For women at high risk, low-dose aspirin has been shown to reduce the risk of developing pre-eclampsia when started early in pregnancy. Maintaining a healthy weight, controlling blood pressure, and managing any underlying medical conditions can also help reduce the risk. Regular prenatal care is essential for all pregnant women, as it allows for the early detection of pre-eclampsia and timely intervention.Living with Pre-Eclampsia
Coping with Pre-Eclampsia
Coping with a diagnosis of pre-eclampsia can be challenging, both physically and emotionally. It is essential for women to have a support system in place and to communicate openly with their healthcare providers about their concerns and feelings. Joining a support group, either in person or online, can provide a sense of community and help women feel less isolated. Practicing stress-reducing techniques, such as meditation or deep breathing, can also help manage the emotional aspects of the condition.Future Research Directions
Conclusion and Next Steps
In conclusion, pre-eclampsia is a significant complication of pregnancy that requires careful management to prevent serious consequences for both the mother and the baby. By understanding the risk factors, recognizing the symptoms, and following the recommended management strategies, women can reduce their risk of developing pre-eclampsia and ensure the best possible outcomes if the condition does occur. It is crucial for pregnant women and their families to be informed and proactive in their prenatal care, working closely with healthcare providers to monitor for signs of pre-eclampsia and to manage the condition effectively if it arises.What are the symptoms of pre-eclampsia?
+The symptoms of pre-eclampsia can include high blood pressure, protein in the urine, severe headaches, vision changes, and abdominal pain. In severe cases, it can lead to seizures (eclampsia) and other complications.
How is pre-eclampsia diagnosed?
+Pre-eclampsia is diagnosed based on the new onset of hypertension and proteinuria after 20 weeks of gestation. Blood pressure and urine tests are used to confirm the diagnosis.
Can pre-eclampsia be prevented?
+While there is no guaranteed way to prevent pre-eclampsia, certain measures can reduce the risk, such as maintaining a healthy weight, controlling blood pressure, and managing underlying medical conditions. Low-dose aspirin has also been shown to reduce the risk in high-risk women.
We hope this comprehensive overview of pre-eclampsia has provided valuable insights and information for expectant mothers and their families. By understanding this condition and taking proactive steps in prenatal care, women can work towards a healthy pregnancy and a positive outcome for both themselves and their babies. If you have any questions or concerns about pre-eclampsia or any other aspect of pregnancy care, we encourage you to reach out to your healthcare provider. Sharing this article with others can also help spread awareness about pre-eclampsia and its importance in pregnancy care.
