Intro
Discover key facts about Prostate Antigen Test, including PSA levels, prostate cancer screening, and biopsy procedures, to understand prostate health and diagnostic techniques.
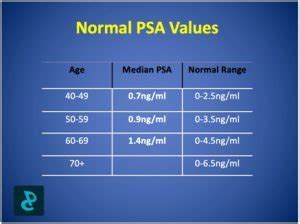
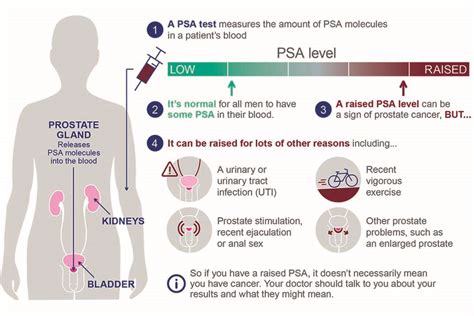
The prostate-specific antigen (PSA) test has been a cornerstone in the diagnosis and management of prostate health for decades. This simple blood test measures the level of PSA, a protein produced by the prostate gland, in the blood. Elevated PSA levels can indicate prostate cancer, but they can also be caused by other factors. As such, understanding the nuances of the PSA test is crucial for men, particularly those over the age of 50, to make informed decisions about their health.
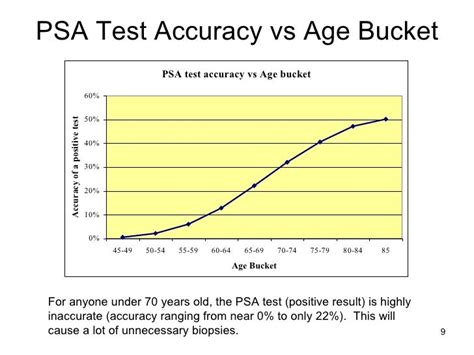
The importance of the PSA test cannot be overstated. Prostate cancer is one of the most common cancers among men, and early detection significantly improves treatment outcomes. However, the test is not without controversy. There have been debates about its effectiveness, the risk of false positives, and the potential for overdiagnosis and overtreatment. Despite these challenges, the PSA test remains a valuable tool in the fight against prostate cancer.
As medical science continues to evolve, so does our understanding of the PSA test and its role in prostate health. Recent studies have highlighted the importance of considering other factors alongside PSA levels, such as family history, ethnicity, and overall health, to get a more accurate picture of an individual's risk. Moreover, advancements in diagnostic technologies, such as MRI scans and genetic testing, are providing healthcare providers with more precise tools to detect and manage prostate cancer.
Understanding the PSA Test
How the PSA Test Works
The PSA test is relatively straightforward. A blood sample is taken from the patient, usually from a vein in the arm, and sent to a laboratory for analysis. The results are then compared to a standard range to determine if the PSA level is elevated. It's worth noting that PSA levels can fluctuate over time and may be influenced by various factors, including certain medications, recent prostate procedures, or even bike riding, which can cause temporary inflammation of the prostate.Benefits of the PSA Test

Early Detection and Treatment
Early detection through the PSA test allows for timely intervention, which can include active surveillance, surgery, radiation therapy, or other treatments, depending on the stage and aggressiveness of the cancer. Active surveillance, for example, involves closely monitoring the cancer with regular PSA tests, digital rectal exams, and biopsies, avoiding or delaying treatment and its potential side effects unless there are signs that the cancer is progressing.Risks and Limitations of the PSA Test
Overdiagnosis and Overtreatment
Another significant issue is the risk of overdiagnosis and overtreatment. Overdiagnosis refers to the detection of cancers that are so slow-growing they would never cause symptoms or death. Overtreatment occurs when these cancers are treated aggressively, potentially leading to unnecessary side effects such as incontinence and impotence. This dilemma underscores the importance of careful consideration and discussion between patients and healthcare providers about the benefits and risks of screening and treatment.Improving the Accuracy of the PSA Test
Multi-Parametric MRI and Genetic Testing
Another significant advancement is the use of multi-parametric MRI scans, which can provide detailed images of the prostate and help identify suspicious areas that may require a biopsy. Genetic testing, such as analyzing for inherited mutations in genes like BRCA2, can also provide valuable information about an individual's risk of developing aggressive prostate cancer.Current Recommendations and Guidelines
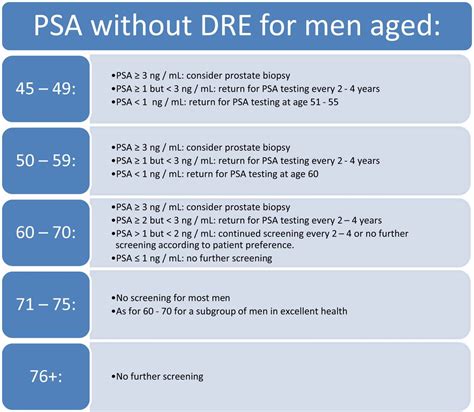
Personalized Approach to Screening
A personalized approach to screening, taking into account individual risk factors, preferences, and values, is increasingly recognized as the best practice. This approach acknowledges that the decision to undergo PSA screening is complex and should be tailored to each man's unique situation.Future Directions in Prostate Cancer Screening
Advancements in Diagnostic Technologies
Advancements in diagnostic technologies, including artificial intelligence and machine learning algorithms to analyze imaging and biomarker data, may also play a significant role in enhancing the accuracy and efficiency of prostate cancer screening. These technologies have the potential to help identify high-risk patients more effectively and reduce unnecessary procedures.Conclusion and Next Steps

Empowering Men's Health
Empowering men with the knowledge and tools to take control of their prostate health is essential. This includes staying informed about the latest developments in screening and treatment, maintaining a healthy lifestyle, and engaging in open discussions with healthcare providers about individual risk factors and screening options.What is the primary purpose of the PSA test?
+The primary purpose of the PSA test is to detect prostate cancer early, when it is more treatable, by measuring the level of prostate-specific antigen in the blood.
What are the risks associated with the PSA test?
+The PSA test is associated with risks such as false positives, which can lead to unnecessary anxiety, biopsies, and treatments, as well as overdiagnosis and overtreatment of slow-growing cancers that may never cause symptoms or death.
How often should men get a PSA test?
+The frequency of PSA testing depends on individual risk factors and should be discussed with a healthcare provider. Generally, men with average risk may start discussing screening at age 50, while those at higher risk may need to start earlier.
What are the benefits of early detection of prostate cancer?
+Early detection of prostate cancer through the PSA test and other diagnostic methods can significantly improve treatment outcomes and survival rates, as well as provide options for less invasive treatments.
How can men reduce their risk of prostate cancer?
+While there is no guaranteed way to prevent prostate cancer, men can reduce their risk by maintaining a healthy diet, staying physically active, not smoking, and limiting alcohol consumption. Regular screening and discussing individual risk factors with a healthcare provider are also crucial.
We invite you to share your thoughts and experiences regarding the PSA test and prostate health. Your insights can help others make informed decisions about their health. Please comment below or share this article with someone who might benefit from this information. Together, we can promote awareness and support for men's health initiatives.
