Intro
Discover how short acting insulin works to manage blood sugar levels, regulating glucose uptake, and preventing hyperglycemia with rapid onset, peak, and duration, improving diabetes control and overall health outcomes.
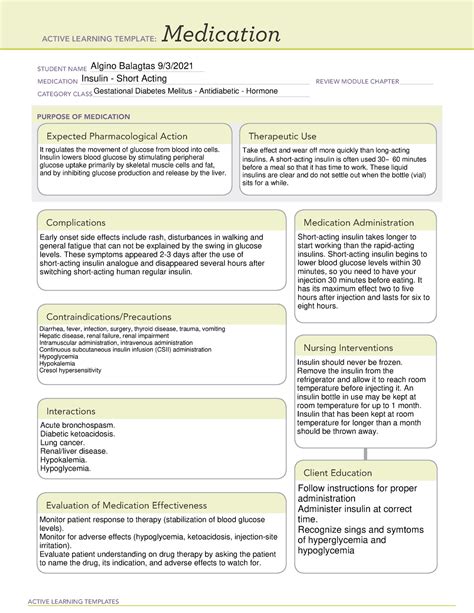
The importance of insulin in the human body cannot be overstated, particularly for individuals living with diabetes. Insulin is a hormone that regulates blood sugar levels, ensuring that glucose is properly absorbed and utilized by cells throughout the body. For those with diabetes, insulin therapy is often a crucial component of their treatment plan. One type of insulin that plays a significant role in managing blood glucose levels is short-acting insulin. In this article, we will delve into the world of short-acting insulin, exploring how it works, its benefits, and what individuals can expect when using this type of insulin.
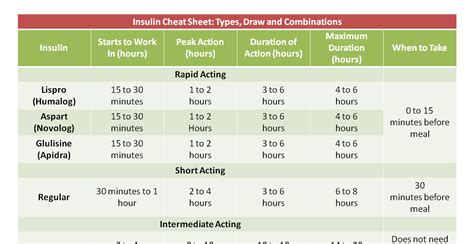
Understanding the different types of insulin is essential for effective diabetes management. Insulin can be categorized based on its onset and duration of action. Short-acting insulin, as the name suggests, begins to work quickly after administration and has a shorter duration of action compared to other types of insulin. This characteristic makes it particularly useful for managing blood sugar spikes that occur after meals. By understanding how short-acting insulin works, individuals with diabetes can better navigate their condition and make informed decisions about their care.
The mechanism of action of short-acting insulin is straightforward yet highly effective. After administration, typically through injection, short-acting insulin begins to lower blood glucose levels by facilitating the uptake of glucose into cells. This process not only helps to regulate postprandial (after meal) glucose spikes but also prevents the accumulation of glucose in the bloodstream, which can lead to various complications if left unchecked. The quick onset of action of short-acting insulin allows for its administration shortly before meals, providing a flexible and effective way to manage meal-related glucose fluctuations.
Benefits of Short Acting Insulin

How to Use Short Acting Insulin
Using short-acting insulin effectively requires an understanding of its administration and dosing. The dosage of short-acting insulin is typically determined based on the individual's current blood glucose level, the size and carbohydrate content of the meal about to be consumed, and their personal insulin sensitivity. It's crucial to work closely with a healthcare provider to determine the correct dosage and to learn how to adjust it based on changing circumstances, such as variations in meal size or physical activity levels.Types of Short Acting Insulin
Rapid Acting vs. Short Acting Insulin
The distinction between rapid-acting and short-acting insulin is important. While both types are used to manage postprandial glucose spikes, rapid-acting insulins have a faster onset of action, typically starting to work within 15 minutes of administration, and may have a slightly shorter duration of action. This rapid onset can be beneficial for individuals who experience significant glucose spikes after meals and need quick action to manage these spikes. However, the choice between rapid-acting and traditional short-acting insulin should be made in consultation with a healthcare provider, considering individual needs and preferences.Side Effects of Short Acting Insulin
Managing Side Effects
Managing the side effects of short-acting insulin involves a combination of proper dosing, monitoring of blood glucose levels, and awareness of the signs and symptoms of hypoglycemia and other side effects. It's essential to work closely with a healthcare provider to adjust insulin dosages and to develop strategies for managing side effects. This may include adjusting meal sizes and content, increasing physical activity, and being vigilant about monitoring blood glucose levels, especially after administering insulin.Living with Short Acting Insulin

Long-Term Management
Long-term management of diabetes with short-acting insulin involves ongoing monitoring and adjustments. Over time, insulin sensitivity and needs may change, requiring adjustments to dosages. Regular check-ups with a healthcare provider are essential to assess the effectiveness of the current treatment plan and make any necessary adjustments. Additionally, staying informed about new developments in insulin therapy and diabetes management can help individuals make the most of their treatment plan and improve their overall health and well-being.Future of Short Acting Insulin

Emerging Technologies
Emerging technologies, such as continuous glucose monitoring systems and smart insulin pens, are also expected to play a significant role in the future of diabetes management. These technologies can provide real-time data on glucose levels and insulin dosages, enabling more precise and personalized management of diabetes. Furthermore, advancements in artificial intelligence and machine learning may lead to the development of predictive models that can forecast glucose levels and recommend optimal insulin dosages, further improving the effectiveness of short-acting insulin therapy.What is the primary benefit of using short-acting insulin?
+The primary benefit of using short-acting insulin is its flexibility, allowing for administration shortly before meals and adjusting dosages based on meal size and content.
How does short-acting insulin work?
+Short-acting insulin works by facilitating the uptake of glucose into cells, thus lowering blood glucose levels. It is typically administered before meals to manage postprandial glucose spikes.
What are the common side effects of short-acting insulin?
+Common side effects of short-acting insulin include hypoglycemia (low blood sugar), injection site reactions, and weight gain. Monitoring blood glucose levels and adjusting dosages as needed can help manage these side effects.
Can short-acting insulin be used in conjunction with other types of insulin?
+Yes, short-acting insulin can be used in conjunction with other types of insulin, such as long-acting insulin, as part of a basal-bolus insulin regimen. This approach can provide both background insulin coverage and meal-time glucose control.
How can I learn more about short-acting insulin and its use in diabetes management?
+To learn more about short-acting insulin, consult with your healthcare provider or a diabetes educator. They can provide personalized guidance and recommendations based on your specific needs and health status.
In conclusion, short-acting insulin is a powerful tool in the management of diabetes, offering flexibility, effectiveness, and the potential for a more normal lifestyle. By understanding how short-acting insulin works, its benefits, and how to use it effectively, individuals with diabetes can better manage their condition and improve their overall health and well-being. We invite you to share your experiences or ask questions about short-acting insulin in the comments below, and to share this article with anyone who might benefit from this information. Together, we can work towards better diabetes management and a healthier future for all.
