Intro
Identify preeclampsia signs and symptoms, including high blood pressure, proteinuria, and swelling, to ensure timely pregnancy care and prevent complications like eclampsia and HELLP syndrome.
Preeclampsia is a pregnancy complication that can have severe consequences for both the mother and the baby if left untreated. It is a condition characterized by high blood pressure and often accompanied by significant amounts of protein in the urine. This condition typically develops after 20 weeks of gestation and can lead to premature birth, low birth weight, and other complications. Understanding the signs and symptoms of preeclampsia is crucial for early detection and management, which can significantly improve outcomes for both mother and baby.
The importance of recognizing preeclampsia signs cannot be overstated. High blood pressure during pregnancy can lead to damage in various organs such as the kidneys, liver, brain, and eyes. In severe cases, it can cause seizures, a condition known as eclampsia, which is a significant threat to the life of both the mother and the fetus. Moreover, preeclampsia is a leading cause of maternal and fetal morbidity and mortality worldwide, emphasizing the need for vigilant monitoring and prompt intervention.
Preeclampsia can affect any pregnant woman, although some are at higher risk than others. Women who are pregnant for the first time, those carrying multiple fetuses, and women with a history of high blood pressure, kidney disease, or certain autoimmune disorders are at increased risk. Given the potential severity of preeclampsia, it is essential for all pregnant women to be aware of the signs and symptoms and to attend regular prenatal check-ups where their blood pressure and urine protein levels can be monitored.
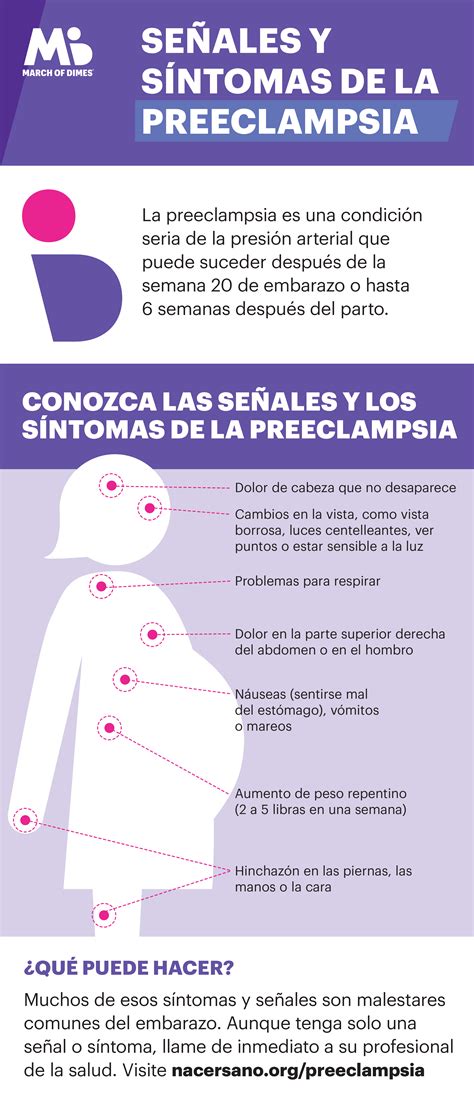
Preeclampsia Signs and Symptoms

The signs and symptoms of preeclampsia can vary from woman to woman and may resemble those of other conditions, making early detection challenging. Common symptoms include high blood pressure, proteinuria (excess protein in the urine), severe headaches, vision changes (such as double vision, blurring, or sensitivity to light), nausea and vomiting, abdominal pain, and decreased urine output. In some cases, women with preeclampsia may not exhibit noticeable symptoms, which is why regular prenatal care is critical for early detection.
Understanding High Blood Pressure in Pregnancy
High blood pressure, or hypertension, is a key indicator of preeclampsia. Blood pressure is considered high in pregnancy if it exceeds 140/90 mmHg. Women with pre-existing hypertension are at a higher risk of developing preeclampsia. Monitoring blood pressure regularly during prenatal visits allows healthcare providers to identify any changes that may indicate the onset of preeclampsia.Risk Factors for Preeclampsia
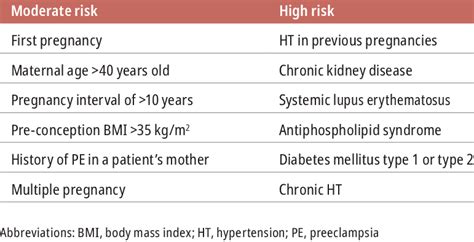
Several factors increase a woman's risk of developing preeclampsia. These include first pregnancy, age 35 or older, carrying twins or other multiples, history of preeclampsia in a previous pregnancy, pre-existing high blood pressure, kidney disease, or autoimmune disorders like lupus, and obesity. Women with a family history of preeclampsia are also at higher risk. Understanding these risk factors can help women and their healthcare providers be more vigilant for signs of preeclampsia.
Diagnosing Preeclampsia
Diagnosing preeclampsia involves a combination of clinical evaluation, laboratory tests, and sometimes imaging studies. Healthcare providers look for high blood pressure and protein in the urine. Additional tests may include blood tests to assess liver and kidney function and ultrasound to evaluate fetal well-being. In some cases, a non-stress test or biophysical profile may be performed to assess the baby's movement and well-being.Treatment and Management of Preeclampsia
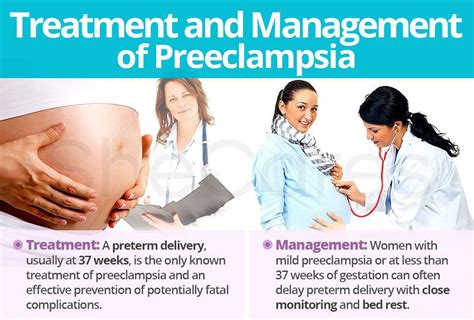
The management of preeclampsia depends on the severity of the condition and the gestational age of the fetus. For women with mild preeclampsia, close monitoring of blood pressure and fetal well-being may be sufficient. This often involves more frequent prenatal visits and may include bed rest. In more severe cases, hospitalization may be necessary to closely monitor the mother and the baby. Corticosteroids may be given to promote fetal lung maturity if preterm delivery is considered. In severe cases, delivery, either vaginally or by cesarean section, may be the only cure for preeclampsia.
Prevention Strategies
While preeclampsia cannot be completely prevented, certain strategies may reduce the risk. These include maintaining a healthy weight before and during pregnancy, following a balanced diet, engaging in regular physical activity as advised by a healthcare provider, and attending all scheduled prenatal appointments. For women at high risk, low-dose aspirin may be recommended starting early in pregnancy to reduce the risk of developing preeclampsia.Complications of Preeclampsia
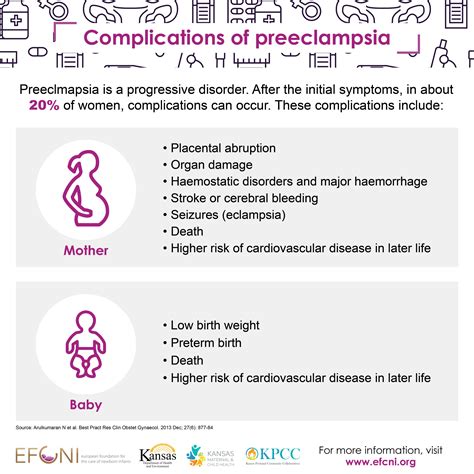
Preeclampsia can lead to several complications for both the mother and the baby. For the mother, potential complications include eclampsia (seizures), stroke, kidney and liver damage, and placental abruption (where the placenta separates from the uterus). For the baby, complications can include premature birth, low birth weight, and restricted growth due to inadequate nutrition and oxygen supply. In severe cases, preeclampsia can lead to stillbirth.
Support and Resources
Women diagnosed with preeclampsia and their families may need emotional support and access to resources. Healthcare providers can offer guidance and connect patients with support groups and educational materials. Online resources and patient organizations can also provide valuable information and a sense of community.Long-term Implications of Preeclampsia
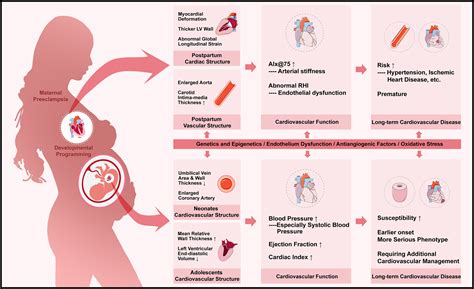
Preeclampsia can have long-term implications for women's health. Women who have had preeclampsia are at a higher risk of developing high blood pressure and cardiovascular disease later in life. Therefore, it is essential for these women to maintain a healthy lifestyle, including a balanced diet, regular exercise, and monitoring of their blood pressure.
Future Pregnancies
For women who have experienced preeclampsia in a previous pregnancy, the risk of developing it again in a future pregnancy is increased. However, with close monitoring and appropriate management, many women can have healthy subsequent pregnancies. It is crucial for these women to discuss their history of preeclampsia with their healthcare provider before becoming pregnant again.Conclusion and Next Steps
In conclusion, preeclampsia is a significant pregnancy complication that requires vigilance and prompt management. Understanding the signs, symptoms, and risk factors can help in early detection and treatment. Women who have experienced preeclampsia should be aware of the potential long-term implications for their health and take steps to maintain a healthy lifestyle.
We invite you to share your experiences or questions about preeclampsia in the comments below. If you found this information helpful, please consider sharing it with others who may benefit from knowing more about this important pregnancy complication. Together, we can work towards better health outcomes for mothers and babies worldwide.
What are the primary symptoms of preeclampsia?
+The primary symptoms of preeclampsia include high blood pressure, excess protein in the urine, severe headaches, vision changes, and abdominal pain.
How is preeclampsia diagnosed?
+Preeclampsia is diagnosed through a combination of clinical evaluation, laboratory tests (such as blood and urine tests), and sometimes imaging studies to assess fetal well-being.
Can preeclampsia be prevented?
+While preeclampsia cannot be completely prevented, certain strategies such as maintaining a healthy weight, following a balanced diet, engaging in regular physical activity, and attending all prenatal appointments can reduce the risk.
What are the potential long-term implications of preeclampsia for women's health?
+Women who have had preeclampsia are at a higher risk of developing high blood pressure and cardiovascular disease later in life, emphasizing the importance of long-term health monitoring and maintenance of a healthy lifestyle.
Is preeclampsia more likely to occur in subsequent pregnancies?
+Yes, women who have experienced preeclampsia in a previous pregnancy are at an increased risk of developing it again in a future pregnancy, although close monitoring and appropriate management can help ensure a healthy outcome.
