Intro
Understand the progressive Stages Of Renal Failure, including acute kidney injury, chronic kidney disease, and end-stage renal disease, to manage symptoms and slow disease progression effectively.
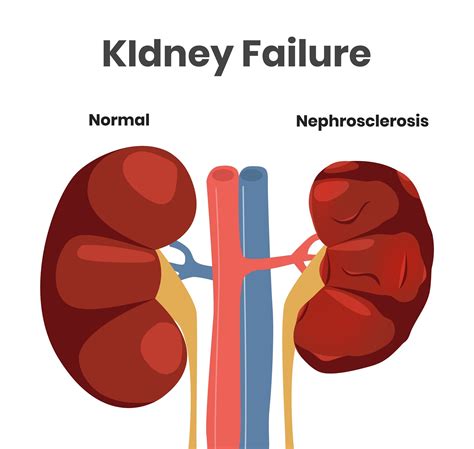
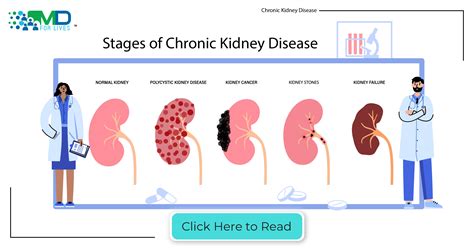
Renal failure, also known as kidney failure, is a serious medical condition that occurs when the kidneys are no longer able to perform their normal functions. The kidneys play a crucial role in filtering waste and excess fluids from the blood, regulating blood pressure, and maintaining electrolyte balance. When the kidneys fail, it can lead to a buildup of toxins and waste products in the body, causing a range of symptoms and complications. Understanding the stages of renal failure is essential for diagnosis, treatment, and management of the condition.
Renal failure can be acute or chronic, with each type having distinct causes, symptoms, and treatment options. Acute renal failure occurs suddenly, often as a result of injury, infection, or medication, and can be reversible with prompt treatment. Chronic renal failure, on the other hand, is a gradual process that can take months or years to develop, often as a result of underlying medical conditions such as diabetes, hypertension, or kidney disease. Recognizing the stages of renal failure is critical for healthcare providers to develop effective treatment plans and for patients to manage their condition and prevent further progression.
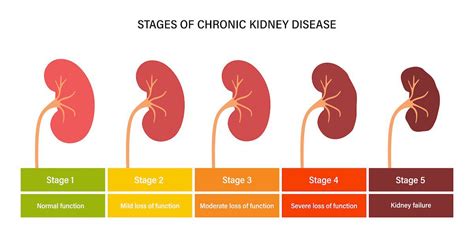
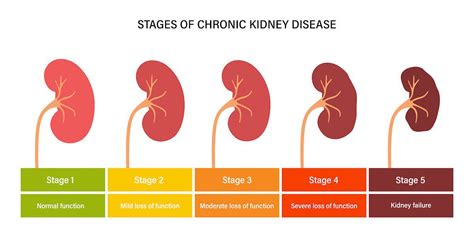
The progression of renal failure can be divided into five stages, each characterized by a decline in kidney function and an increase in waste products in the blood. The stages of renal failure are based on the glomerular filtration rate (GFR), which measures the rate at which the kidneys filter waste and excess fluids from the blood. Understanding the stages of renal failure is essential for patients and healthcare providers to work together to manage the condition, slow disease progression, and improve quality of life.
Stage 1: Kidney Damage with Normal Kidney Function
Stage 2: Kidney Damage with Mild Loss of Kidney Function
Treatment Options for Stage 2 Kidney Disease
Treatment for stage 2 kidney disease focuses on managing underlying medical conditions, such as hypertension or diabetes, and reducing proteinuria. Medications, such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), may be prescribed to slow disease progression and reduce proteinuria. Patients should also work with their healthcare providers to develop a comprehensive treatment plan, including lifestyle modifications and regular monitoring of kidney function.Stage 3: Moderate Loss of Kidney Function
Complications of Stage 3 Kidney Disease
Stage 3 kidney disease increases the risk of complications, such as cardiovascular disease, anemia, and bone disease. Patients should work closely with their healthcare providers to manage these complications and prevent further progression of kidney disease. Regular monitoring of kidney function, electrolyte levels, and blood pressure is essential to prevent complications and ensure timely intervention.Stage 4: Severe Loss of Kidney Function
Preparing for Kidney Replacement Therapy
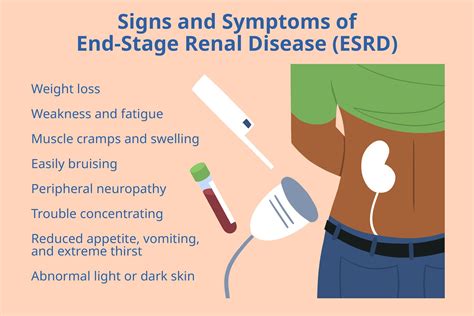
Patients with stage 4 kidney disease should begin preparing for kidney replacement therapy, such as dialysis or transplantation. This includes education on treatment options, vascular access creation, and transplantation evaluation. Patients should also work with their healthcare providers to manage symptoms, prevent complications, and ensure timely intervention.Stage 5: End-Stage Renal Disease (ESRD)
Treatment Options for ESRD
Treatment options for ESRD include hemodialysis, peritoneal dialysis, and kidney transplantation. Patients should work closely with their healthcare providers to determine the best treatment option and develop a comprehensive treatment plan. Regular monitoring of kidney function, electrolyte levels, and blood pressure is essential to prevent complications and ensure timely intervention.What are the symptoms of renal failure?
+Symptoms of renal failure may include fatigue, weakness, shortness of breath, swelling, and changes in urination patterns.
How is renal failure diagnosed?
+Renal failure is diagnosed through a combination of physical examination, medical history, laboratory tests, and imaging studies.
What are the treatment options for renal failure?
+Treatment options for renal failure include lifestyle modifications, medications, dialysis, and kidney transplantation.
Can renal failure be prevented?
+While some cases of renal failure cannot be prevented, lifestyle modifications, such as maintaining a healthy diet and exercising regularly, can help reduce the risk of developing kidney disease.
What is the prognosis for patients with renal failure?
+The prognosis for patients with renal failure depends on the underlying cause, stage of disease, and treatment options. With proper treatment and management, many patients with renal failure can lead active and fulfilling lives.
In conclusion, understanding the stages of renal failure is essential for patients and healthcare providers to work together to manage the condition, slow disease progression, and improve quality of life. By recognizing the symptoms, causes, and treatment options for each stage, patients can take an active role in managing their condition and preventing further progression. We invite readers to share their experiences, ask questions, and seek guidance from healthcare professionals to better understand the stages of renal failure and develop effective treatment plans.
