Intro
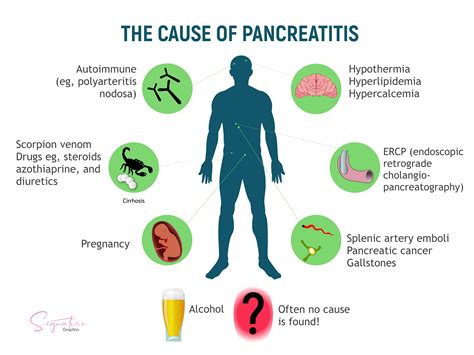
Discover the causes of pancreatitis, including gallstones, alcohol abuse, and genetic factors, and learn about symptoms, diagnosis, and treatment options for this inflammatory condition affecting the pancreas and digestive system.
Pancreatitis, an inflammation of the pancreas, is a complex and potentially life-threatening condition that affects millions of people worldwide. The pancreas, a vital organ located behind the stomach, plays a crucial role in digestion and blood sugar regulation. When the pancreas becomes inflamed, it can cause severe abdominal pain, nausea, vomiting, and even life-threatening complications. Understanding the causes of pancreatitis is essential for prevention, diagnosis, and treatment. In this article, we will delve into the various causes of pancreatitis, exploring the risk factors, symptoms, and consequences of this condition.
The pancreas is a delicate organ that can be affected by a range of factors, including genetics, lifestyle, and environmental factors. Pancreatitis can be acute or chronic, with acute pancreatitis being a sudden and short-term inflammation, while chronic pancreatitis is a long-term and recurring condition. Both forms of pancreatitis can have significant consequences on a person's quality of life, making it essential to understand the underlying causes. By recognizing the risk factors and symptoms of pancreatitis, individuals can take proactive steps to prevent the condition and seek medical attention if symptoms persist.
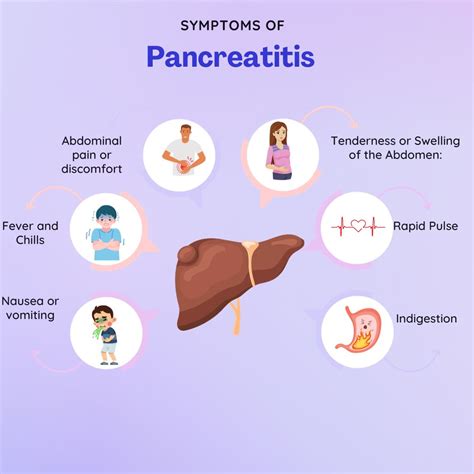
Pancreatitis is often associated with severe abdominal pain, which can radiate to the back and worsen after eating. Other symptoms include nausea, vomiting, fever, and abdominal tenderness. If left untreated, pancreatitis can lead to serious complications, such as pancreatic necrosis, infection, and even organ failure. The economic burden of pancreatitis is also significant, with hospitalization and treatment costs running into thousands of dollars. Furthermore, pancreatitis can have a profound impact on a person's mental and emotional well-being, causing anxiety, depression, and stress. By understanding the causes of pancreatitis, we can work towards preventing and managing this condition, reducing its economic and emotional toll on individuals and society.
Introduction to Pancreatitis Causes
Genetic Mutations and Pancreatitis
Genetic mutations can also play a role in the development of pancreatitis. Certain genetic disorders, such as cystic fibrosis, can increase the risk of pancreatitis. Additionally, mutations in the PRSS1 gene can cause hereditary pancreatitis, a rare but severe form of the condition. Other genetic mutations, such as those affecting the SPINK1 gene, can also increase the risk of pancreatitis. Understanding the genetic basis of pancreatitis is essential for developing targeted therapies and preventive strategies.Risk Factors for Pancreatitis
Medications and Pancreatitis
Certain medications can increase the risk of pancreatitis, either by causing direct pancreatic damage or by triggering an allergic reaction. These medications include: * Corticosteroids: Long-term use of corticosteroids can increase the risk of pancreatitis. * Antibiotics: Certain antibiotics, such as tetracyclines and sulfonamides, can increase the risk of pancreatitis. * Chemotherapy: Certain chemotherapy agents can cause pancreatic damage and increase the risk of pancreatitis. * Azathioprine: This immunosuppressive medication can increase the risk of pancreatitis.Diagnosis and Treatment of Pancreatitis
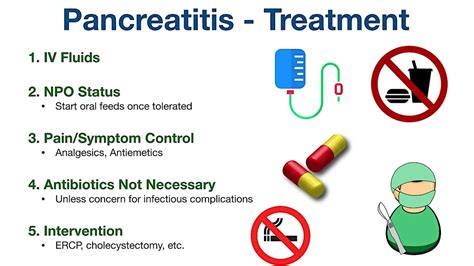
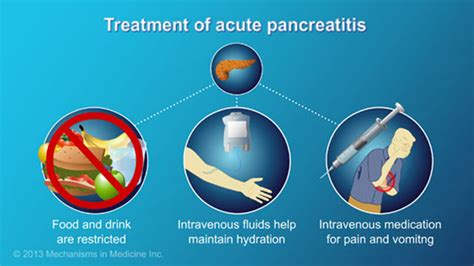
Treatment Options for Pancreatitis
Treatment options for pancreatitis include: * Pain management: Medications such as opioids and NSAIDs can help manage pain. * Hydration: Intravenous fluids can help replenish fluids and electrolytes. * Nutritional support: Patients may require nutritional support, such as enteral or parenteral nutrition. * Antibiotics: If an infection is present, antibiotics may be prescribed. * Surgery: In severe cases, surgical intervention may be necessary to remove damaged pancreatic tissue or repair any complications.Prevention and Management of Pancreatitis
Lifestyle Modifications for Pancreatitis Prevention
Lifestyle modifications can play a significant role in preventing pancreatitis. These include: * Quitting smoking * Avoiding fatty foods * Increasing physical activity * Managing stress * Getting enough sleepConclusion and Future Directions

As we continue to learn more about pancreatitis, it is essential to raise awareness about this condition and its impact on individuals and society. By working together, we can reduce the burden of pancreatitis and improve the lives of those affected by this condition. If you or someone you know is experiencing symptoms of pancreatitis, it is essential to seek medical attention promptly. With proper diagnosis and treatment, it is possible to manage pancreatitis and prevent long-term complications.
We invite you to share your thoughts and experiences with pancreatitis in the comments below. Your input can help us better understand this condition and develop more effective strategies for prevention and management. Additionally, we encourage you to share this article with others who may be affected by pancreatitis, helping to raise awareness and promote education about this important health topic.
What are the symptoms of pancreatitis?
+The symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, fever, and abdominal tenderness. In severe cases, pancreatitis can cause complications such as pancreatic necrosis, infection, and organ failure.
How is pancreatitis diagnosed?
+Pancreatitis is typically diagnosed using a combination of physical examination, laboratory tests, and imaging studies. Blood tests can help identify elevated pancreatic enzymes, while imaging studies such as CT scans and ultrasound can help visualize the pancreas and detect any abnormalities.
Can pancreatitis be prevented?
+Yes, pancreatitis can be prevented by addressing the underlying risk factors and taking proactive steps to reduce the risk of developing the condition. This includes maintaining a healthy weight, eating a balanced diet, avoiding excessive alcohol consumption, managing diabetes and high triglycerides, and avoiding certain medications.
What are the treatment options for pancreatitis?
+Treatment options for pancreatitis depend on the underlying cause and severity of the condition. Mild cases may be managed with supportive care, such as pain management and hydration, while more severe cases may require hospitalization and surgical intervention.
Can pancreatitis be managed with lifestyle modifications?
+Yes, lifestyle modifications can play a significant role in managing pancreatitis. This includes quitting smoking, avoiding fatty foods, increasing physical activity, managing stress, and getting enough sleep. Additionally, maintaining a healthy weight, eating a balanced diet, and avoiding excessive alcohol consumption can help reduce the risk of developing pancreatitis.
