Intro
Discover Phenobarbitals uses, effects, and interactions. Learn about its role in seizure control, anxiety relief, and insomnia treatment, as well as potential side effects and withdrawal symptoms.
The world of medicine is filled with a wide array of drugs, each designed to treat specific conditions or symptoms. Among these, phenobarbital stands out as a medication with a rich history and diverse applications. Phenobarbital, also known as phenobarbitone, is a barbiturate that has been used for nearly a century in the treatment of various health issues. Its uses range from controlling seizures and epilepsy to managing insomnia and anxiety, showcasing its versatility in the medical field. Understanding the uses and effects of phenobarbital is crucial for both medical professionals and patients alike, as it can significantly impact treatment outcomes and patient well-being.
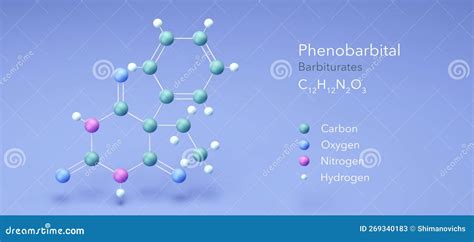
Phenobarbital's mechanism of action involves enhancing the activity of gamma-aminobutyric acid (GABA), a neurotransmitter in the brain that inhibits nerve transmissions, thereby producing a calming effect on the nervous system. This action underlies its therapeutic effects in conditions characterized by excessive neuronal activity, such as epilepsy. Moreover, its sedative properties make it useful for treating insomnia and restlessness. The drug's long history of use has also led to its application in other areas, including as an emergency treatment for seizures and as part of the management regimen for status epilepticus, a severe and potentially life-threatening condition.
The importance of phenobarbital in modern medicine cannot be overstated, given its efficacy and the breadth of its applications. Despite the development of newer antiepileptic drugs, phenobarbital remains a valuable option, especially in resource-limited settings where access to more recent medications may be restricted. Its use, however, must be carefully managed due to potential side effects and the risk of dependence. Understanding these aspects is vital for healthcare providers to ensure that patients receive the most appropriate treatment while minimizing risks.
Introduction to Phenobarbital

Phenobarbital is classified as a barbiturate, a class of drugs known for their sedative and hypnotic effects. It was first synthesized in the early 20th century and quickly found its place in clinical practice due to its potent anticonvulsant properties. Over the years, its use has evolved, reflecting changes in medical understanding and the development of new therapeutic agents. Today, phenobarbital is recognized for its efficacy in treating a range of neurological conditions, including epilepsy, seizure disorders, and, in some cases, anxiety and sleep disorders.
History of Phenobarbital
The history of phenobarbital is intertwined with the broader narrative of barbiturate development. Initially hailed as a breakthrough in the treatment of insomnia and anxiety, barbiturates soon found applications in managing seizure disorders. Phenobarbital, with its favorable pharmacokinetic profile, became a preferred choice among barbiturates for its antiepileptic properties. Its use peaked in the mid-20th century, after which newer, safer antiepileptic drugs began to emerge, gradually replacing phenobarbital in many clinical settings. However, its legacy continues, and it remains an essential drug in many parts of the world.Pharmacology of Phenobarbital
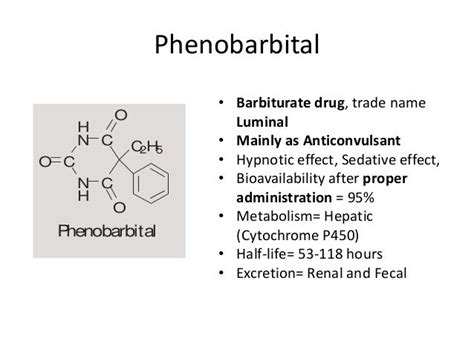
The pharmacological profile of phenobarbital is characterized by its ability to act on the central nervous system (CNS), enhancing the effect of GABA, the primary inhibitory neurotransmitter in the brain. This action results in a reduction of neuronal excitability, which underlies its anticonvulsant and sedative effects. Phenobarbital is well absorbed orally, achieves peak plasma concentrations within a few hours, and has a half-life that allows for once or twice daily dosing, making it convenient for long-term management of chronic conditions.
Metabolism and Excretion
Phenobarbital is metabolized in the liver, primarily through the cytochrome P450 system, and its metabolites are excreted in the urine. This metabolic pathway is significant because it can lead to drug interactions, particularly with other drugs that induce or inhibit the cytochrome P450 enzymes. Understanding these interactions is crucial for avoiding adverse effects and ensuring the efficacy of phenobarbital and co-administered medications.Therapeutic Uses of Phenobarbital
Phenobarbital's therapeutic applications are diverse, reflecting its sedative, anticonvulsant, and anxiolytic properties. The primary uses include:
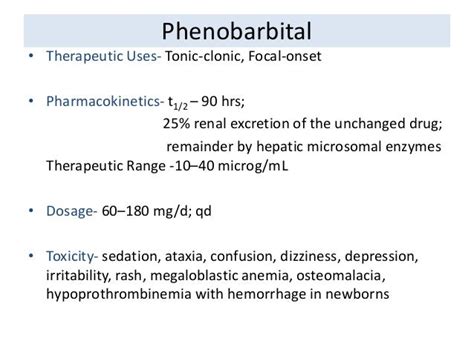
- Epilepsy and Seizure Disorders: Phenobarbital is effective in controlling various types of seizures, including tonic-clonic, partial, and status epilepticus.
- Insomnia and Sleep Disorders: Its sedative effects make it useful for treating insomnia, although its use for this indication has declined with the availability of safer alternatives.
- Anxiety and Restlessness: Phenobarbital can be used to manage anxiety and restlessness, particularly in situations where a rapid onset of action is desired.
Benefits and Risks
While phenobarbital offers significant benefits in the management of certain medical conditions, its use is also associated with risks, including dependence, withdrawal symptoms upon cessation, and potential for overdose. The risk of dependence is a critical consideration, as it can limit the drug's long-term utility and lead to complications upon withdrawal. Therefore, phenobarbital should be prescribed judiciously, with careful monitoring of patients for signs of dependence or other adverse effects.Side Effects and Interactions
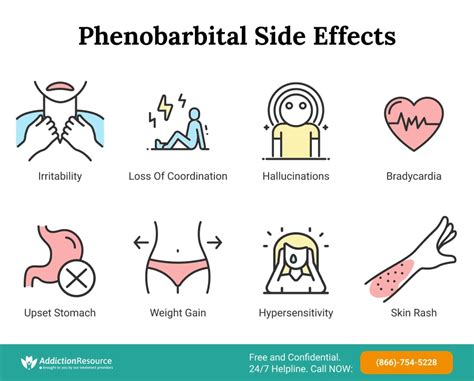
The side effect profile of phenobarbital includes drowsiness, dizziness, ataxia, and cognitive impairment. More severe side effects can occur, such as Stevens-Johnson syndrome, a rare but potentially life-threatening condition. Phenobarbital also interacts with a wide range of drugs, affecting their metabolism and increasing the risk of adverse effects. Common interactions include those with other CNS depressants, which can enhance sedative effects, and with drugs metabolized by the cytochrome P450 system, which can lead to altered plasma concentrations of either phenobarbital or the co-administered drug.
Management of Side Effects
Managing the side effects of phenobarbital involves careful dose adjustment, monitoring for signs of toxicity, and consideration of alternative treatments when necessary. In cases of overdose, supportive care and, in severe instances, the use of activated charcoal or other interventions to reduce drug absorption may be required. The potential for dependence and withdrawal necessitates a gradual tapering of the dose when discontinuing phenobarbital, under close medical supervision.Dosage and Administration
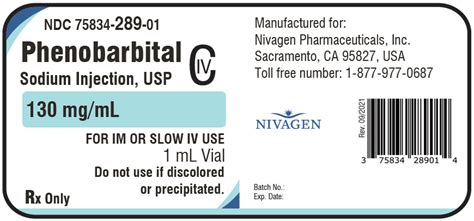
The dosage of phenobarbital varies depending on the indication, patient age, and other factors. For epilepsy, for example, the dose may range from 60 to 200 mg per day, given in divided doses. The sedative effects of phenobarbital are dose-dependent, with higher doses required for hypnotic effects. It is essential to follow the prescribed dosing regimen closely to minimize the risk of adverse effects while achieving therapeutic efficacy.
Special Considerations
Special considerations are necessary when prescribing phenobarbital to certain patient populations, including the elderly, pregnant women, and individuals with liver or kidney dysfunction. The drug's metabolism and excretion may be altered in these groups, necessitating dose adjustments to avoid toxicity. Furthermore, the risk of dependence and the potential for drug interactions must be carefully weighed against the benefits of treatment.Patient Education and Counseling
Educating patients about the proper use of phenobarbital, its potential side effects, and the importance of adherence to the prescribed regimen is crucial. Patients should be advised about the risks of dependence and the need for gradual dose tapering when discontinuing the medication. Additionally, they should be informed about potential drug interactions and the importance of reporting any changes in their medication regimen to their healthcare provider.
Future Directions
The future of phenobarbital in clinical practice will likely be shaped by ongoing research into its pharmacology and therapeutic applications. Despite the availability of newer antiepileptic drugs, phenobarbital remains a valuable option, particularly in settings where access to these newer agents is limited. Continued studies into its safety profile, efficacy, and potential new uses will help to refine its role in modern medicine.Conclusion and Final Thoughts
In conclusion, phenobarbital is a medication with a rich history and diverse therapeutic applications. Its use in managing epilepsy, insomnia, and anxiety reflects its versatility and efficacy. However, its potential for dependence and side effects necessitates careful management and patient education. As medical science continues to evolve, the role of phenobarbital will likely continue to adapt, reflecting new understandings of its pharmacology and the development of new therapeutic agents.
What is phenobarbital used for?
+Phenobarbital is used for the treatment of epilepsy, seizure disorders, insomnia, and anxiety. It acts as a sedative and anticonvulsant, making it useful for managing a range of neurological conditions.
How does phenobarbital work?
+Phenobarbital works by enhancing the effect of gamma-aminobutyric acid (GABA), a neurotransmitter in the brain that inhibits nerve transmissions, thereby producing a calming effect on the nervous system.
What are the potential side effects of phenobarbital?
+The potential side effects of phenobarbital include drowsiness, dizziness, ataxia, cognitive impairment, and the risk of dependence and withdrawal symptoms. More severe side effects, such as Stevens-Johnson syndrome, can also occur.
We hope this comprehensive overview of phenobarbital has provided valuable insights into its uses, effects, and management. Whether you are a healthcare professional or a patient, understanding the complexities of this medication can help ensure its safe and effective use. Feel free to share your thoughts or ask questions in the comments below, and don't forget to share this article with anyone who might benefit from this information. Together, let's continue the conversation about the importance of informed healthcare practices.
