Intro
Discover the comprehensive Beta Blockers List, featuring medications like propranolol and atenolol, used to treat hypertension, angina, and heart failure, with related LSI keywords: blood pressure, cardiovascular, and beta blockers side effects.
The use of beta blockers has become a cornerstone in the management of various cardiovascular conditions, including hypertension, angina, heart failure, and arrhythmias. These medications work by blocking the effects of the hormone epinephrine, also known as adrenaline, and by slowing the heart rate and reducing its workload. This action helps to lower blood pressure, reduce the heart's oxygen demand, and improve survival in patients with heart failure. With the numerous benefits they offer, it's essential to understand the different types of beta blockers available, their mechanisms of action, and their applications in clinical practice.
The development of beta blockers has a rich history, dating back to the 1960s when the first beta blocker, propranolol, was introduced. Since then, numerous beta blockers have been developed, each with its unique properties and uses. Understanding the differences between these medications can help healthcare providers and patients make informed decisions about their treatment plans. Moreover, the evolution of beta blockers has led to the development of more selective and targeted therapies, reducing side effects and improving patient outcomes.
The importance of beta blockers in modern medicine cannot be overstated. They have revolutionized the treatment of cardiovascular diseases, significantly reducing morbidity and mortality. By controlling heart rate and blood pressure, beta blockers can prevent complications such as heart attacks, strokes, and sudden cardiac death. Furthermore, their use has been expanded to other areas, including the management of performance anxiety, migraines, and glaucoma. As research continues to uncover the benefits and potential applications of beta blockers, their role in healthcare is likely to expand further.
Beta Blockers Classification
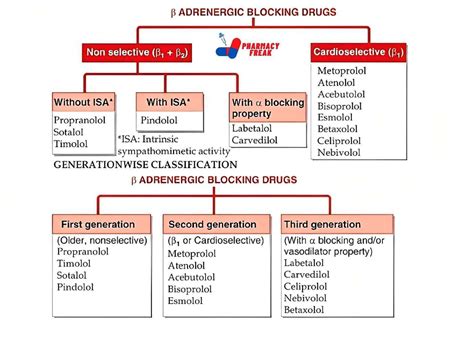
Non-Selective Beta Blockers
Non-selective beta blockers, such as propranolol and nadolol, block both beta-1 and beta-2 adrenergic receptors. This broad action can be beneficial in certain conditions but also increases the risk of side effects, particularly in patients with asthma or chronic obstructive pulmonary disease (COPD). The use of non-selective beta blockers requires careful consideration of the patient's overall health status and the presence of any comorbidities.Types of Beta Blockers
Benefits of Beta Blockers
The benefits of beta blockers are numerous and well-documented. They include: - Reduced blood pressure: Beta blockers decrease the heart's workload and output, leading to lower blood pressure. - Decreased heart rate: By slowing the heart rate, beta blockers reduce the heart's oxygen demand, which can help in managing angina and improving survival in heart failure. - Improved heart function: In patients with heart failure, beta blockers can improve the heart's pumping efficiency and reduce the risk of complications. - Reduced risk of heart attack and stroke: By controlling blood pressure and heart rate, beta blockers can significantly reduce the risk of cardiovascular events.Side Effects of Beta Blockers

Contraindications and Precautions
Beta blockers are contraindicated in certain conditions, such as: - Uncontrolled heart failure - Cardiogenic shock - Severe bradycardia - Hypotension - Asthma and COPD (for non-selective beta blockers) Additionally, caution is advised when using beta blockers in patients with diabetes, as they can mask symptoms of hypoglycemia and affect glucose metabolism.Interactions with Other Medications
Dosage and Administration
The dosage of beta blockers varies depending on the specific medication, the patient's condition, and their response to the treatment. It's crucial to follow the prescribed dosage and administration instructions carefully to minimize side effects and maximize benefits. Additionally, patients should not stop taking beta blockers abruptly, as this can lead to withdrawal symptoms and a rebound effect.Future Perspectives

Conclusion and Recommendations
In conclusion, beta blockers are a vital class of medications in the management of cardiovascular diseases. Their ability to reduce morbidity and mortality, combined with their relatively favorable side effect profile, makes them an indispensable tool in modern medicine. Patients and healthcare providers must work together to ensure that beta blockers are used effectively and safely, taking into account the individual's health status, potential side effects, and interactions with other medications. By doing so, we can maximize the benefits of beta blockers and improve outcomes for those affected by cardiovascular diseases.What are beta blockers used for?
+Beta blockers are used for a variety of conditions, including hypertension, angina, heart failure, arrhythmias, and to prevent heart attacks and strokes.
How do beta blockers work?
+Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline, and by slowing the heart rate and reducing its workload.
What are the common side effects of beta blockers?
+Common side effects of beta blockers include fatigue, dizziness, cold hands and feet, shortness of breath, and sexual dysfunction.
Can I stop taking beta blockers abruptly?
+No, patients should not stop taking beta blockers abruptly, as this can lead to withdrawal symptoms and a rebound effect. It's essential to consult with a healthcare provider before making any changes to the medication regimen.
How can I minimize the side effects of beta blockers?
+To minimize side effects, patients should follow the prescribed dosage, report any side effects to their healthcare provider, and avoid stopping the medication abruptly.
We hope this comprehensive overview of beta blockers has provided valuable insights into their mechanisms, benefits, and potential applications. Whether you're a healthcare provider looking to improve patient outcomes or an individual seeking to understand your treatment options better, the information presented here aims to empower you with the knowledge necessary to make informed decisions about beta blockers. If you have any further questions or would like to share your experiences with beta blockers, please don't hesitate to comment or share this article with others who might find it helpful. Together, we can work towards better health outcomes for all.
