Intro
Learn about retained placenta symptoms, causes, and treatment. Identify signs of placental retention, such as bleeding and uterine pain, and understand complications like infection and hemorrhage.
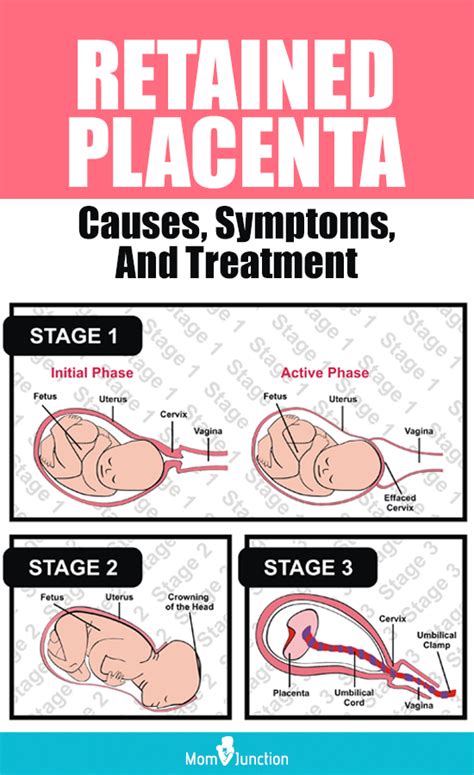
Retained placenta is a serious medical condition that can occur after childbirth, where the placenta fails to deliver spontaneously within a reasonable timeframe, typically 30 minutes to 1 hour after the birth of the baby. This condition can lead to severe bleeding, infection, and other complications if left untreated. It is essential for new mothers to be aware of the symptoms of retained placenta to seek medical attention promptly.
The placenta plays a vital role in the development of the fetus during pregnancy, providing oxygen and nutrients and removing waste products. After childbirth, the placenta is expected to separate from the uterus and deliver spontaneously. However, in some cases, the placenta may not separate or deliver completely, leading to a retained placenta. This condition can be life-threatening if not treated promptly and effectively.
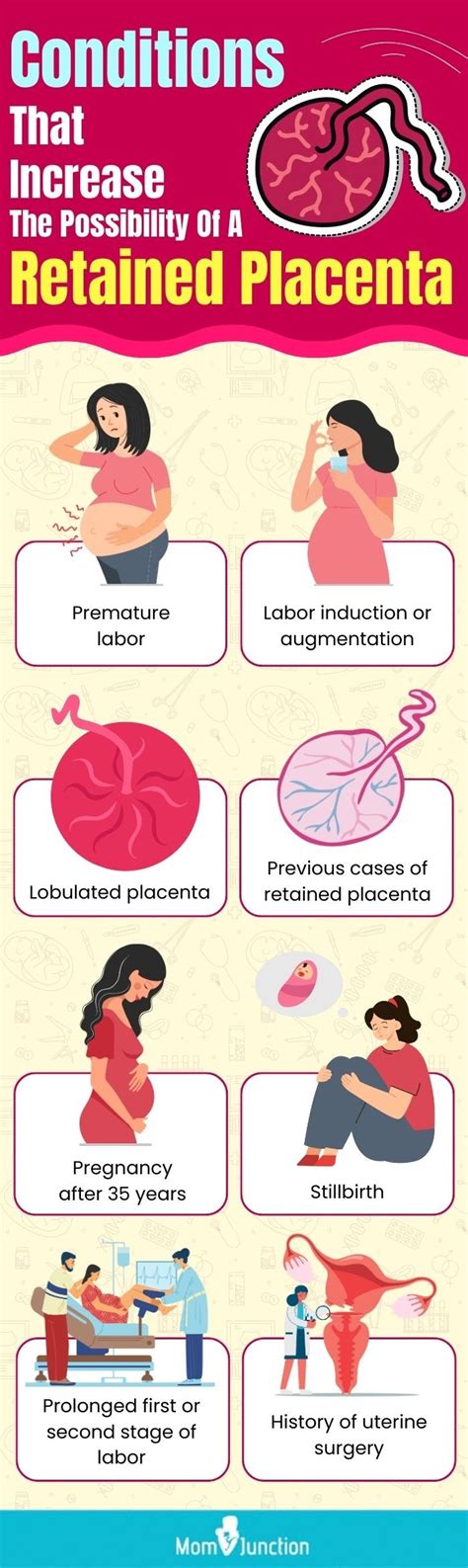
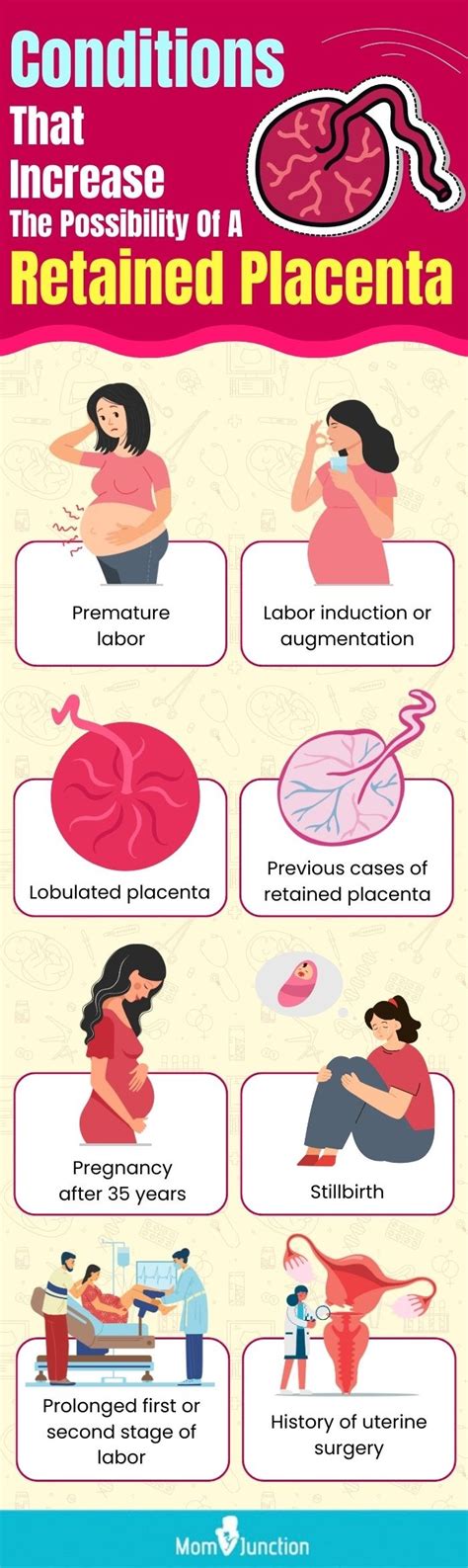
Retained placenta can occur due to various reasons, including uterine atony, where the uterus fails to contract and separate the placenta, or placenta accreta, where the placenta grows too deeply into the uterine wall. Other factors that may contribute to retained placenta include previous uterine surgery, multiple pregnancies, and placental abnormalities. It is crucial for healthcare providers to monitor new mothers closely after childbirth to detect any signs of retained placenta and provide timely interventions.
Causes and Risk Factors
Uterine Factors
Uterine factors are the most common cause of retained placenta, accounting for approximately 80% of cases. Uterine atony is the most significant risk factor, where the uterus fails to contract and separate the placenta. Previous uterine surgery, such as cesarean section or myomectomy, can also increase the risk of retained placenta. Uterine abnormalities, such as uterine fibroids or adenomyosis, can also contribute to retained placenta.Placental Factors
Placental factors are the second most common cause of retained placenta, accounting for approximately 15% of cases. Placenta accreta is a significant risk factor, where the placenta grows too deeply into the uterine wall. Placental abnormalities, such as placental infarction or placental abruption, can also increase the risk of retained placenta. Multiple pregnancies, such as twins or triplets, can also contribute to retained placenta.Symptoms and Diagnosis
Clinical Examination
Clinical examination is the first step in diagnosing retained placenta. Healthcare providers will assess uterine tone, placental separation, and vaginal bleeding. A thorough abdominal examination can help identify uterine tenderness, masses, or other abnormalities. Vaginal examination can help assess placental separation and identify any retained placental tissue.Ultrasound
Ultrasound is a valuable tool in diagnosing retained placenta. Transabdominal or transvaginal ultrasound can help visualize the placenta and assess its separation from the uterus. Ultrasound can also help identify any retained placental tissue or blood clots. In some cases, ultrasound may be used to guide manual removal of the placenta or other interventions.Treatment and Management
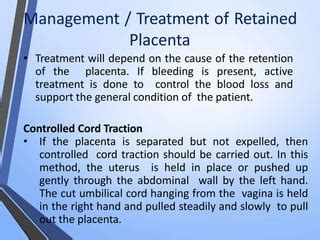
Conservative Management
Conservative management of retained placenta involves uterine massage, oxytocin infusion, and close monitoring. Uterine massage can help stimulate uterine contractions and promote placental separation. Oxytocin infusion can help stimulate uterine contractions and reduce bleeding. Close monitoring is essential to assess uterine tone, placental separation, and vaginal bleeding.Surgical Interventions
Surgical interventions may be necessary in more severe cases of retained placenta. Manual removal of the placenta involves gently removing the placenta from the uterus. Uterine evacuation involves removing any retained placental tissue or blood clots from the uterus. In some cases, women may require a hysterectomy or other surgical procedures to manage severe bleeding or infection.Complications and Prevention
Severe Bleeding
Severe bleeding is a significant complication of retained placenta. Women may experience heavy vaginal bleeding, which can lead to hypovolemic shock, organ failure, and even death. Prompt treatment with uterine massage, oxytocin infusion, and blood transfusions can help manage bleeding and prevent complications.Infection
Infection is another significant complication of retained placenta. Women may experience fever, chills, and signs of infection, which can lead to sepsis, organ failure, and even death. Prompt treatment with antibiotics and supportive care can help manage infection and prevent complications.What are the symptoms of retained placenta?
+The symptoms of retained placenta include severe bleeding, abdominal pain, and uterine tenderness. In some cases, women may experience fever, chills, or signs of infection.
How is retained placenta diagnosed?
+Diagnosis of retained placenta is typically made through clinical examination, ultrasound, and laboratory tests. Healthcare providers may perform a physical examination to assess uterine tone and placental separation. Ultrasound can help confirm the diagnosis by visualizing the placenta and assessing its separation from the uterus.
What are the complications of retained placenta?
+Complications of retained placenta can be severe and life-threatening if left untreated. Common complications include severe bleeding, infection, and uterine rupture. Prompt treatment with uterine massage, oxytocin infusion, and blood transfusions can help manage bleeding and prevent complications.
In conclusion, retained placenta is a serious medical condition that requires prompt attention and treatment. By understanding the causes, symptoms, and complications of retained placenta, healthcare providers can provide targeted interventions and reduce the risk of severe bleeding, infection, and other complications. Women who have experienced retained placenta can share their experiences and raise awareness about this important health issue. We invite readers to comment, share this article, or take specific actions to promote awareness and education about retained placenta.
