Intro
Learn about Staph A symptoms, causes, and treatments. Understand methicillin-resistant Staphylococcus aureus (MRSA) infections, boils, and cellulitis, and discover how to manage symptoms and prevent spread.
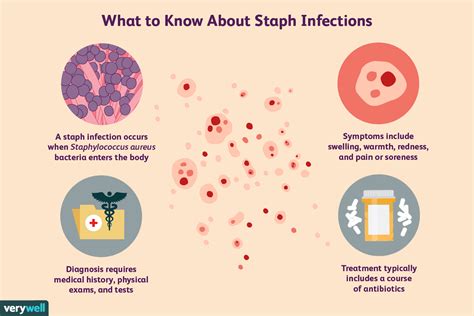
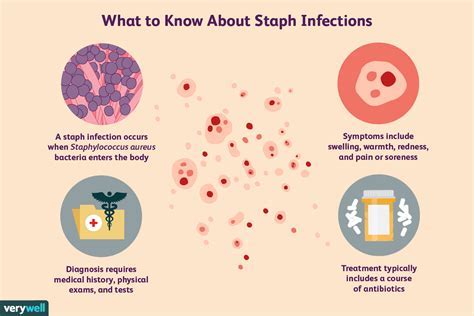
The importance of understanding Staph A symptoms cannot be overstated, as this bacterium is a common cause of infections that can range from mild to severe. Staphylococcus aureus, commonly referred to as Staph A, is a type of bacteria that can be found on the skin and in the noses of healthy individuals. However, when it enters the body through cuts or other openings, it can cause a variety of infections, including skin infections, respiratory tract infections, and even life-threatening conditions such as sepsis and endocarditis. Recognizing the symptoms of Staph A infections is crucial for seeking timely medical attention and preventing the spread of the infection to others.
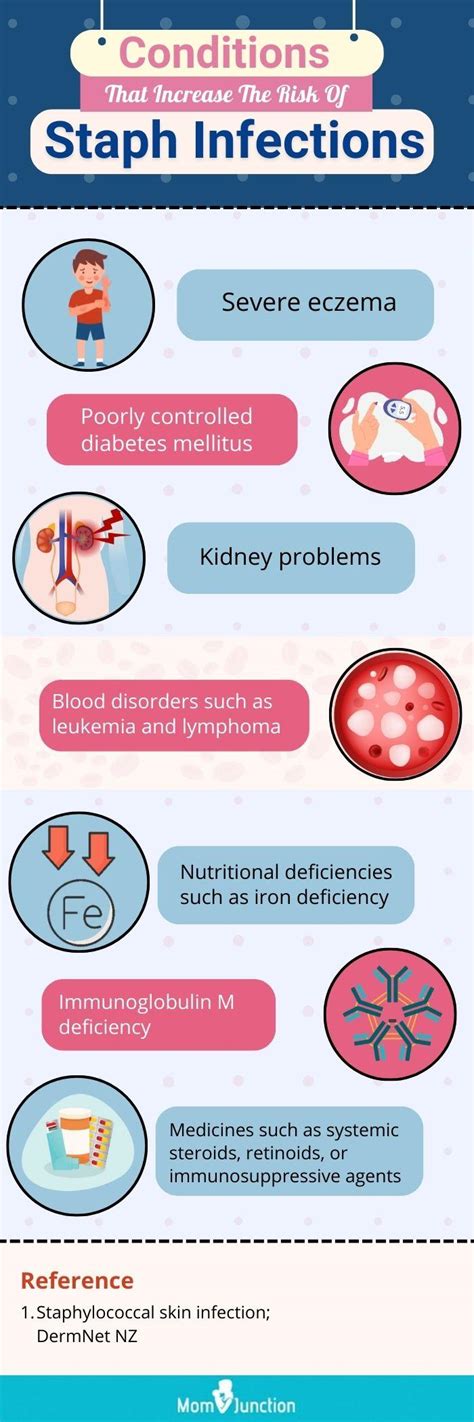
Staph A infections can affect anyone, regardless of age or health status. However, certain individuals are more susceptible to developing severe infections, including young children, older adults, and people with weakened immune systems. The symptoms of Staph A infections can vary depending on the location and severity of the infection. For example, skin infections may cause redness, swelling, and pus-filled blisters, while respiratory tract infections may cause coughing, fever, and shortness of breath. Understanding the different types of Staph A infections and their symptoms is essential for proper diagnosis and treatment.
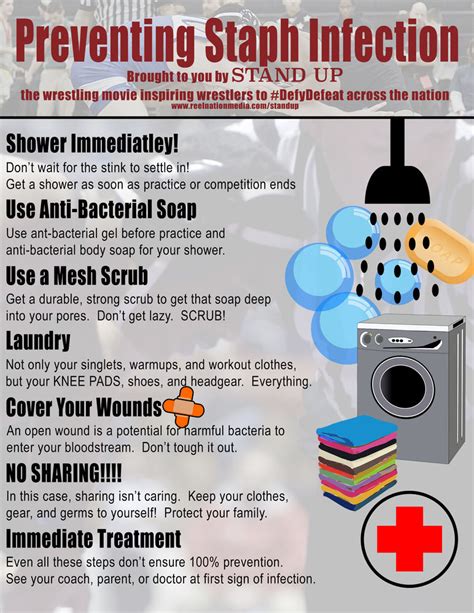
The rise of antibiotic-resistant Staph A strains, such as methicillin-resistant Staphylococcus aureus (MRSA), has made it even more critical to recognize the symptoms of Staph A infections and seek medical attention promptly. MRSA infections can be challenging to treat and may require specialized care. Furthermore, the spread of Staph A infections can be prevented through proper hygiene practices, such as frequent handwashing and covering wounds. By understanding the symptoms and prevention strategies, individuals can take proactive steps to protect themselves and their loved ones from the risks associated with Staph A infections.
Understanding Staph A Infections
Types of Staph A Infections
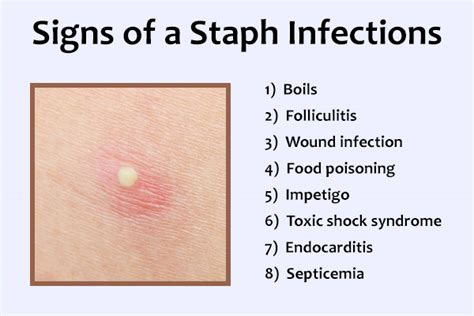
The different types of Staph A infections include: * Skin and soft tissue infections, such as impetigo, folliculitis, and cellulitis * Respiratory tract infections, such as pneumonia and bronchitis * Bloodstream infections, such as sepsis and endocarditis * Bone and joint infections, such as osteomyelitis and septic arthritis * Gastrointestinal infections, such as food poisoning and gastroenteritisRecognizing Staph A Symptoms
Diagnosing Staph A Infections
Diagnosing Staph A infections typically involves a combination of physical examination, medical history, and laboratory tests. Laboratory tests may include: * Blood cultures to detect the presence of bacteria in the bloodstream * Urine tests to detect the presence of bacteria in the urine * Imaging tests, such as X-rays and CT scans, to visualize the infection site * Biopsy to examine tissue samples for signs of infectionPreventing Staph A Infections
Managing Staph A Infections
Managing Staph A infections typically involves a combination of antibiotics, wound care, and supportive care. Antibiotics may be prescribed to treat the infection, while wound care may involve cleaning and dressing the wound to promote healing. Supportive care may include rest, hydration, and pain management.Treating Staph A Infections

Antibiotic Resistance and Staph A Infections
The rise of antibiotic-resistant Staph A strains, such as MRSA, has made it challenging to treat Staph A infections. MRSA infections may require specialized care, including intravenous antibiotics and hospitalization. Preventing the spread of antibiotic-resistant Staph A strains requires proper hygiene practices, infection control measures, and responsible use of antibiotics.Complications of Staph A Infections
Long-Term Effects of Staph A Infections
The long-term effects of Staph A infections can be significant, especially if left untreated or inadequately treated. Some possible long-term effects include: * Scarring and disfigurement from skin and soft tissue infections * Chronic pain and disability from bone and joint infections * Increased risk of future infections and complications * Emotional and psychological trauma from severe or life-threatening infectionsConclusion and Next Steps
We invite you to share your thoughts and experiences with Staph A infections in the comments below. If you have any questions or concerns, please do not hesitate to reach out. By working together, we can raise awareness and promote prevention and treatment of Staph A infections.
What are the common symptoms of Staph A infections?
+Common symptoms of Staph A infections include redness and swelling at the site of infection, pus-filled blisters or abscesses, fever and chills, coughing and shortness of breath, diarrhea and vomiting, and abdominal pain and cramping.
How can I prevent Staph A infections?
+Preventing Staph A infections requires a combination of proper hygiene practices, wound care, and infection control measures. Some ways to prevent Staph A infections include practicing good hygiene, covering wounds and cuts, avoiding close contact with individuals who have Staph A infections, and keeping surfaces and equipment clean and disinfected.
What are the complications of Staph A infections?
+Complications of Staph A infections can be severe and even life-threatening. Some possible complications include sepsis, endocarditis, osteomyelitis, septic arthritis, and abscesses.
