Intro
Discover 5 ways to interpret TB test results, understanding tuberculosis diagnosis, symptoms, and treatment options, with insights on Mantoux test, IGRA, and chest X-rays for accurate TB detection and management.
The importance of understanding TB test results cannot be overstated, especially for individuals who have been exposed to tuberculosis or are at high risk of contracting the disease. Tuberculosis, a bacterial infection caused by Mycobacterium tuberculosis, can be a serious health threat if left undiagnosed or untreated. The first step in managing TB is to undergo a diagnostic test, and interpreting the results correctly is crucial for effective treatment and prevention of further spread. In this article, we will delve into the various aspects of TB test results, exploring what they mean, how they are interpreted, and the implications for individuals and public health.
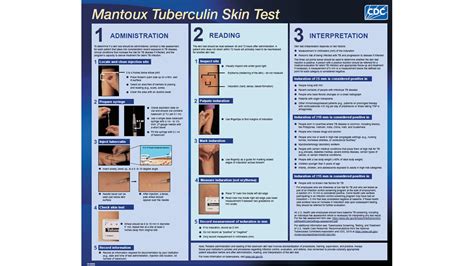
TB testing is a critical tool in the fight against tuberculosis, allowing healthcare providers to identify infected individuals, initiate treatment, and prevent the spread of the disease. There are several types of TB tests, including the Mantoux tuberculin skin test (TST), interferon-gamma release assays (IGRAs), and molecular tests like the Xpert MTB/RIF assay. Each test has its own strengths and limitations, and understanding these differences is essential for accurate interpretation of test results.
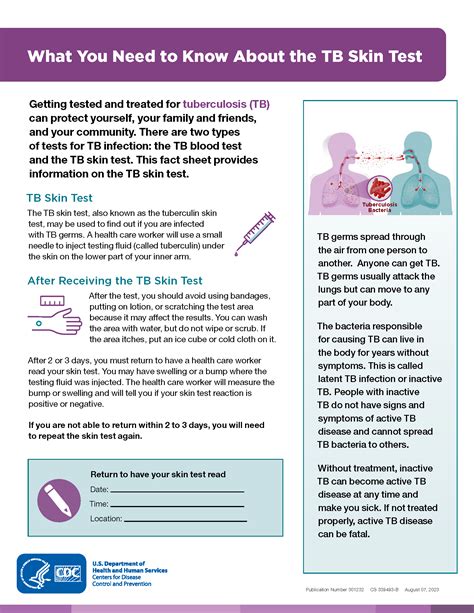
The process of interpreting TB test results involves several steps, including assessing the individual's risk factors, considering the type of test used, and evaluating the results in the context of clinical symptoms and medical history. For instance, a positive result on a TST or IGRA may indicate that an individual has been infected with TB, but it does not necessarily mean they have active disease. On the other hand, a negative result does not entirely rule out the possibility of TB infection, especially in individuals with weakened immune systems or those who have recently been exposed to the bacteria.
Understanding TB Test Results
Understanding TB test results is crucial for individuals who have undergone testing, as well as for healthcare providers who must interpret these results and make informed decisions about treatment and care. The results of TB tests can be categorized into several types, including positive, negative, and indeterminate. A positive result typically indicates that an individual has been infected with TB, although it may not distinguish between latent and active disease. A negative result suggests that the individual is not infected, but this can be influenced by various factors, such as the timing of the test, the individual's immune status, and the type of test used.
Types of TB Tests
The choice of TB test depends on several factors, including the individual's risk factors, medical history, and the availability of testing resources. The most commonly used tests include: - Mantoux tuberculin skin test (TST): This is the oldest and most widely used method for detecting TB infection. It involves injecting a small amount of tuberculin into the skin and measuring the reaction after 48-72 hours. - Interferon-gamma release assays (IGRAs): These blood tests measure the immune response to TB proteins and are more specific than TST, especially in individuals who have received the BCG vaccine. - Molecular tests: These tests, such as the Xpert MTB/RIF assay, detect the genetic material of TB bacteria in sputum or other specimens, providing rapid diagnosis of active TB.Interpreting TB Test Results

Interpreting TB test results requires a comprehensive approach, considering not only the test outcome but also the individual's clinical presentation, medical history, and epidemiological context. For instance, a positive TST result in an asymptomatic individual may indicate latent TB infection, whereas the same result in a symptomatic individual could suggest active TB disease. The interpretation of IGRA results follows similar principles, with positive results indicating TB infection, although these tests are less affected by BCG vaccination or non-tuberculous mycobacterial infections.
Factors Influencing Test Results
Several factors can influence the accuracy and interpretation of TB test results, including: - Recent exposure to TB: Individuals who have been recently exposed may not yet have developed a positive reaction. - Immune status: People with weakened immune systems, such as those with HIV/AIDS, may have false-negative results. - BCG vaccination: This can cause a positive TST result, although the effect diminishes over time. - Non-tuberculous mycobacterial infections: These can also lead to positive TST results, although IGRAs are more specific for TB.Implications of TB Test Results
The implications of TB test results are far-reaching, affecting not only the individual's health and treatment plan but also public health strategies for disease control and prevention. A diagnosis of active TB disease necessitates immediate initiation of antibiotic treatment, typically a combination of four drugs, to cure the disease and prevent transmission to others. Individuals with latent TB infection may be offered preventive therapy to reduce the risk of progression to active disease.
Public Health Implications
From a public health perspective, TB test results are vital for: - Contact tracing: Identifying individuals who have been in close contact with someone diagnosed with active TB. - Outbreak investigations: Understanding the source and spread of TB in communities. - Surveillance: Monitoring TB trends and patterns to inform control and prevention strategies.Management and Treatment
The management and treatment of TB depend on the type of disease (latent or active) and the individual's specific circumstances, such as drug resistance patterns and comorbid conditions. Active TB disease is typically treated with a standard regimen of four antibiotics (isoniazid, rifampicin, pyrazinamide, and ethambutol) for six months, although treatment may be extended in cases of drug-resistant TB or if the individual has certain medical conditions.
Latent TB Infection Treatment
Treatment for latent TB infection is aimed at preventing the progression to active disease and is usually offered to individuals at high risk of developing active TB, such as those with HIV/AIDS or young children. The most commonly used regimen for latent TB infection is isoniazid monotherapy for nine months, although other regimens may be used depending on the individual's circumstances and preferences.Prevention and Control

Prevention and control of TB are multifaceted, involving measures at the individual, community, and societal levels. At the individual level, preventive therapy for latent TB infection and adherence to treatment regimens for active disease are crucial. Community-based initiatives, such as contact tracing and screening programs, can help identify and manage TB cases early, reducing transmission. Societal efforts, including improving living conditions, enhancing healthcare access, and promoting awareness and education about TB, are also vital for controlling the spread of the disease.
Global Efforts
Globally, the World Health Organization (WHO) and other international bodies have set targets to end the TB epidemic by 2030, as part of the Sustainable Development Goals. These efforts include strengthening health systems, improving access to TB diagnosis and treatment, and promoting research into new diagnostic tools, treatments, and vaccines.Future Directions

The future of TB control lies in innovative technologies, enhanced global cooperation, and a patient-centered approach to care. Advances in diagnostic technologies, such as rapid molecular tests and whole-genome sequencing, promise to improve the accuracy and speed of TB diagnosis. New treatments and regimens, including those for drug-resistant TB, are being developed to address the challenges of TB treatment. Moreover, a renewed focus on prevention, through vaccination and other measures, could significantly reduce the global burden of TB.
Research and Development
Ongoing research and development are critical for addressing the gaps in current TB control strategies. This includes the pursuit of a more effective vaccine against TB, the development of shorter, more effective treatment regimens, and the improvement of diagnostic tools to facilitate early detection and treatment of TB.To encourage engagement and action, we invite readers to share their thoughts and experiences with TB testing and treatment. If you or someone you know has been affected by TB, consider reaching out to local health organizations or support groups for information and resources. Together, we can work towards a future where TB is no longer a public health threat.
What does a positive TB test result mean?
+A positive TB test result indicates that an individual has been infected with TB bacteria. However, it does not distinguish between latent and active TB disease.
How is TB treated?
+TB is typically treated with a combination of four antibiotics for six months. The treatment regimen may vary depending on the type of TB (latent or active) and the presence of drug resistance.
Can TB be prevented?
+Yes, TB can be prevented through measures such as BCG vaccination, preventive therapy for latent TB infection, and public health strategies to reduce transmission.
