Intro
Explore ulcerative colitis surgery options, including colectomy, j-pouch, and ostomy, to manage symptoms and improve quality of life with inflammatory bowel disease treatments.
Ulcerative colitis is a chronic condition that causes inflammation and ulceration of the inner lining of the rectum and colon. While medications and lifestyle changes can help manage the symptoms, some people may require surgery to treat the condition. Surgery for ulcerative colitis can be a life-changing decision, and it's essential to understand the different options available. In this article, we will delve into the world of ulcerative colitis surgery options, exploring the benefits, risks, and what to expect from each procedure.
The importance of understanding ulcerative colitis surgery options cannot be overstated. With the rising incidence of the condition, it's crucial to be aware of the various treatment approaches available. Surgery can offer a chance for patients to regain control over their lives, free from the debilitating symptoms of ulcerative colitis. However, it's vital to approach this decision with caution, weighing the pros and cons of each surgical option. As we navigate the complexities of ulcerative colitis surgery, it's essential to consider the latest research, expert opinions, and real-life experiences of patients who have undergone these procedures.
For individuals living with ulcerative colitis, the prospect of surgery can be daunting. The uncertainty surrounding the outcome, the potential risks, and the impact on daily life can be overwhelming. Nevertheless, with the right information and support, patients can make informed decisions about their treatment. As we explore the various ulcerative colitis surgery options, we will examine the latest advancements in surgical techniques, the benefits of minimally invasive procedures, and the importance of post-operative care. Whether you're a patient, a caregiver, or simply looking to learn more about the condition, this article aims to provide a comprehensive guide to ulcerative colitis surgery options.
Introduction to Ulcerative Colitis Surgery
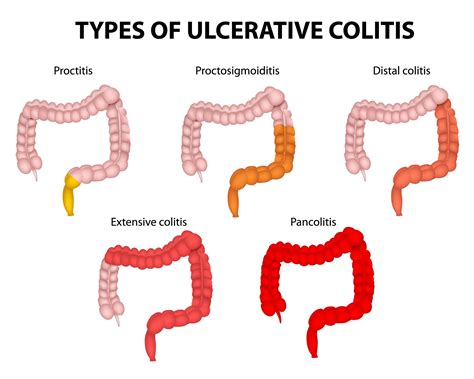
Types of Ulcerative Colitis Surgery
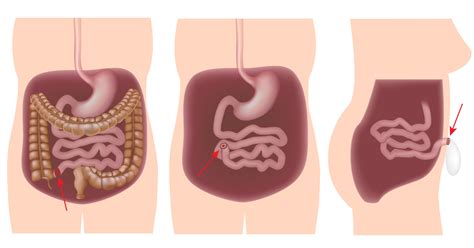
The type of surgery recommended depends on the extent and severity of the disease, as well as the patient's overall health. Some common types of ulcerative colitis surgery include: * Proctocolectomy: This involves the removal of the entire colon and rectum. * Colectomy: This involves the removal of the colon, leaving the rectum intact. * Pouch surgery: This involves creating a pouch from the small intestine to store stool, allowing for more normal bowel function. Each of these surgical options has its own set of benefits and risks, which will be discussed in more detail below.Proctocolectomy with Ileostomy
Risks and Benefits of Proctocolectomy with Ileostomy
The benefits of proctocolectomy with ileostomy include: * Complete removal of the diseased colon and rectum * Significant reduction in symptoms * Improved quality of life However, there are also risks and complications to consider, including: * Infection * Bleeding * Adhesions * Bowel obstruction * Skin irritation and breakdown around the stoma siteColectomy with Ileorectal Anastomosis

Risks and Benefits of Colectomy with Ileorectal Anastomosis
The benefits of colectomy with ileorectal anastomosis include: * Preservation of the rectum and anus * More normal bowel function * Reduced risk of complications compared to proctocolectomy However, there are also risks and complications to consider, including: * Infection * Bleeding * Adhesions * Bowel obstruction * Rectal dysfunctionPouch Surgery
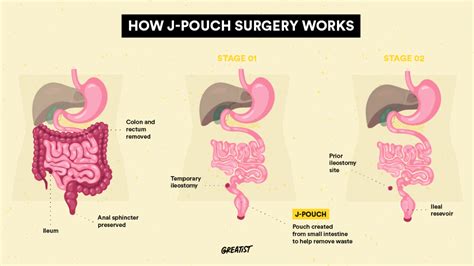
Risks and Benefits of Pouch Surgery
The benefits of pouch surgery include: * Complete removal of the diseased colon and rectum * Preservation of the anus and more normal bowel function * Improved quality of life However, there are also risks and complications to consider, including: * Infection * Bleeding * Adhesions * Bowel obstruction * Pouch dysfunctionMinimally Invasive Surgery

Risks and Benefits of Minimally Invasive Surgery
The benefits of minimally invasive surgery include: * Reduced recovery time * Minimized scarring * Decreased risk of complications * Improved cosmetic results However, there are also risks and complications to consider, including: * Infection * Bleeding * Adhesions * Bowel obstruction * Conversion to open surgeryPost-Operative Care

Importance of Follow-Up Care
Follow-up care is essential for patients undergoing ulcerative colitis surgery. Regular appointments with the surgeon and gastroenterologist can help: * Monitor for complications * Adjust medications * Manage bowel function * Address any concerns or questions By prioritizing follow-up care, patients can ensure the best possible outcomes and reduce the risk of long-term complications.What are the risks and benefits of ulcerative colitis surgery?
+The risks and benefits of ulcerative colitis surgery vary depending on the procedure and individual patient factors. Benefits include significant reduction in symptoms, improved quality of life, and complete removal of the diseased colon and rectum. Risks include infection, bleeding, adhesions, bowel obstruction, and pouch dysfunction.
What is the difference between proctocolectomy and colectomy?
+Proctocolectomy involves the removal of the entire colon and rectum, while colectomy involves the removal of the colon, leaving the rectum intact. The choice of procedure depends on the extent and severity of the disease, as well as individual patient factors.
Can I still have a normal life after ulcerative colitis surgery?
+Yes, many patients are able to lead normal lives after ulcerative colitis surgery. While some procedures may require significant lifestyle adjustments, others can allow for more normal bowel function and improved quality of life. It's essential to discuss individual expectations and outcomes with the surgeon and gastroenterologist.
As we conclude our exploration of ulcerative colitis surgery options, it's essential to remember that each patient's journey is unique. By understanding the different surgical procedures, risks, and benefits, patients can make informed decisions about their treatment. If you or a loved one is considering ulcerative colitis surgery, we encourage you to share your experiences, ask questions, and seek support from healthcare professionals and online communities. Together, we can work towards improving outcomes and enhancing the quality of life for those affected by this condition.
