Intro
Discover 5 essential diuretic facts, exploring natural diuretics, water pills, and fluid retention relief, to help manage bloating and promote healthy urine production.
Diuretics are a class of medications that play a crucial role in managing various health conditions, particularly those related to fluid retention and blood pressure regulation. Understanding how diuretics work and their implications on the body is essential for individuals who are prescribed these medications or are interested in learning more about their health. The importance of diuretics cannot be overstated, as they are a cornerstone in the treatment of conditions such as hypertension, heart failure, and certain kidney and liver diseases.
The mechanism of action of diuretics involves increasing the amount of urine produced by the kidneys, which in turn helps to reduce the volume of fluid in the bloodstream and lower blood pressure. This effect is particularly beneficial for patients with hypertension, as it can help to prevent complications such as heart disease and stroke. Furthermore, diuretics are also used to treat edema, which is the swelling caused by excess fluid trapped in the body's tissues. This condition can be a symptom of various underlying diseases, and the use of diuretics can provide significant relief by reducing the fluid buildup.
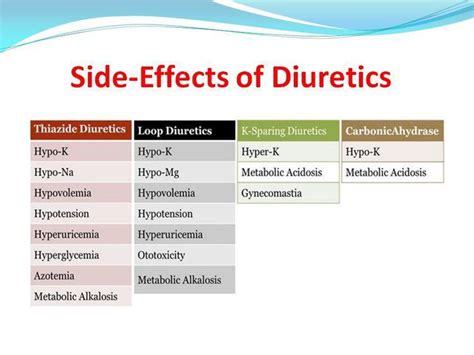
The use of diuretics is not without its considerations, however. Like all medications, diuretics can have side effects, some of which can be significant. Patients taking diuretics need to be aware of the potential for dehydration, electrolyte imbalances, and other effects that can impact their quality of life. Moreover, the management of diuretic therapy requires careful monitoring by healthcare professionals to ensure that the benefits of the medication are maximized while minimizing its risks. This includes regular check-ups, blood tests, and adjustments to the dosage or type of diuretic as necessary.
Introduction to Diuretics
How Diuretics Work
The working mechanism of diuretics is closely related to the kidneys' function of filtering waste and excess fluids from the blood. By enhancing the kidneys' ability to remove fluid, diuretics help in reducing the volume of fluid in the bloodstream, which in turn lowers blood pressure and alleviates edema. This process involves the inhibition of certain transport mechanisms in the renal tubules, leading to increased excretion of sodium, chloride, and water. The reduction in fluid volume not only lowers blood pressure but also decreases the workload on the heart, making diuretics a critical component of heart failure management.Benefits of Diuretics
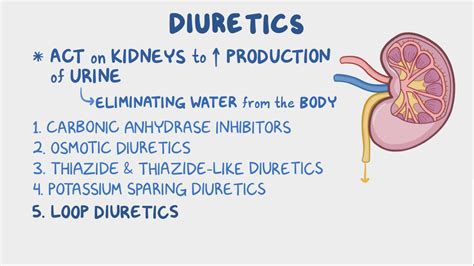
Types of Diuretics
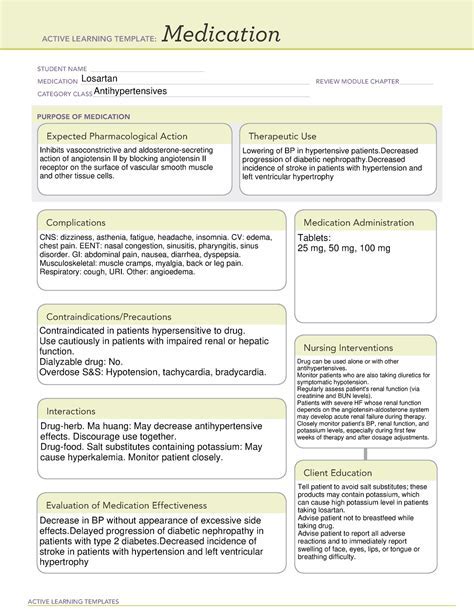
- **Thiazide Diuretics**: Used primarily for hypertension, these diuretics act on the distal convoluted tubule of the nephron. - **Loop Diuretics**: More potent, these are used in edema and in patients with reduced renal function, acting on the ascending limb of the loop of Henle. - **Potassium-Sparing Diuretics**: These have a mild diuretic effect and are used to prevent hypokalemia (low potassium levels), acting on the collecting duct.Side Effects and Considerations
Management and Monitoring
The management of patients on diuretics involves regular monitoring of blood pressure, renal function, and electrolyte levels. This includes periodic blood tests to check for signs of electrolyte imbalance, particularly potassium and sodium levels, and adjustments to the diuretic dose or type as needed. Patients are also advised to maintain a balanced diet, avoid excessive salt intake, and stay hydrated to minimize the risk of dehydration and electrolyte disturbances. In cases where diuretics are used for edema, monitoring for signs of fluid overload or depletion is crucial, and adjustments to therapy are made based on clinical response.Practical Considerations for Patients
Lifestyle Adjustments
Lifestyle adjustments can complement diuretic therapy, enhancing its effectiveness and contributing to overall health. Regular physical activity, a balanced diet, stress management, and avoiding alcohol and tobacco can all play a role in managing conditions for which diuretics are prescribed. Additionally, patients should be aware of the potential for drug interactions with diuretics, particularly with nonsteroidal anti-inflammatory drugs (NSAIDs), which can reduce the effectiveness of diuretics and increase the risk of kidney damage.Future Directions in Diuretic Therapy

Emerging Therapies
Emerging therapies, including novel diuretic compounds and innovative delivery systems, aim to address some of the limitations of current diuretic treatments. These advancements could lead to more personalized treatment approaches, where the choice of diuretic is tailored to the individual patient's needs, potentially improving outcomes and reducing side effects. The integration of diuretic therapy with other treatments, such as device-based therapies for heart failure, also represents a promising area of research, with the potential to offer comprehensive management strategies for complex conditions.What are the primary uses of diuretics in medical practice?
+Diuretics are primarily used to treat conditions such as hypertension (high blood pressure), heart failure, and edema (swelling caused by excess fluid). They work by increasing urine production, which helps reduce fluid volume in the body and lower blood pressure.
How do diuretics affect potassium levels in the body?
+Most diuretics increase the excretion of potassium in the urine, leading to a potential decrease in potassium levels (hypokalemia). This is why some diuretics are classified as potassium-sparing, as they help maintain potassium levels. Patients on diuretic therapy may need regular blood tests to monitor their potassium levels.
Can diuretics be used in patients with kidney disease?
+Yes, diuretics can be used in patients with kidney disease, but their use requires careful consideration and monitoring. The type and dose of diuretic may need to be adjusted based on the patient's renal function, and close monitoring for signs of worsening kidney function or electrolyte imbalances is necessary.
In summary, diuretics play a vital role in the management of various health conditions, offering benefits that can significantly improve patients' quality of life. Understanding how diuretics work, their types, benefits, and potential side effects is essential for maximizing their therapeutic potential. As research continues to advance our understanding of diuretic therapy, patients and healthcare providers can look forward to more effective and safer treatments for conditions that require fluid management. We invite readers to share their experiences or ask questions about diuretics, and we encourage healthcare professionals to contribute their insights into the best practices for diuretic therapy. By engaging in this discussion, we can work together to optimize the use of diuretics and improve patient outcomes.
