Intro
Learn about Type 2 Diabetes, a chronic metabolic disorder characterized by insulin resistance, hyperglycemia, and glucose intolerance, affecting blood sugar levels and overall health, requiring management through diet, exercise, and medication to prevent complications.
Type 2 diabetes is a chronic health condition that affects the way the body processes blood sugar, also known as glucose. It is a complex condition that can have serious consequences if left untreated or poorly managed. In this article, we will delve into the world of type 2 diabetes, exploring its causes, symptoms, diagnosis, treatment options, and management strategies.
Type 2 diabetes is the most common form of diabetes, accounting for about 90% of all diabetes cases. It is a metabolic disorder characterized by high blood sugar levels, which can lead to a range of health problems, including heart disease, kidney damage, and nerve damage. The condition is often associated with insulin resistance, where the body's cells become less responsive to insulin, a hormone produced by the pancreas that regulates blood sugar levels.
The importance of understanding type 2 diabetes cannot be overstated. With the rising prevalence of obesity and physical inactivity, the number of people developing type 2 diabetes is increasing rapidly. According to the World Health Organization (WHO), the number of people living with diabetes has quadrupled since 1980, with an estimated 463 million people affected worldwide. If left unchecked, type 2 diabetes can have devastating consequences, including reduced quality of life, increased healthcare costs, and premature death.
Causes and Risk Factors of Type 2 Diabetes

- Genetics: Family history plays a significant role in the development of type 2 diabetes. Individuals with a first-degree relative (parent or sibling) with type 2 diabetes are more likely to develop the condition.
- Obesity: Excess weight, particularly around the abdominal area, is a major risk factor for type 2 diabetes. This is because excess fat can lead to insulin resistance, making it harder for the body to regulate blood sugar levels.
- Physical inactivity: A sedentary lifestyle can contribute to the development of type 2 diabetes, as regular physical activity helps to improve insulin sensitivity and glucose uptake in the muscles.
- Age: The risk of developing type 2 diabetes increases with age, with most cases occurring in people over the age of 45.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, and Native Americans, are at higher risk of developing type 2 diabetes due to genetic and environmental factors.
Other Risk Factors
In addition to the above factors, other risk factors for type 2 diabetes include: * High blood pressure * High cholesterol * History of gestational diabetes or delivering a baby over 4kg * Polycystic ovary syndrome (PCOS) * Sleep apnea * Certain medications, such as steroids and certain psychiatric medicationsSymptoms of Type 2 Diabetes
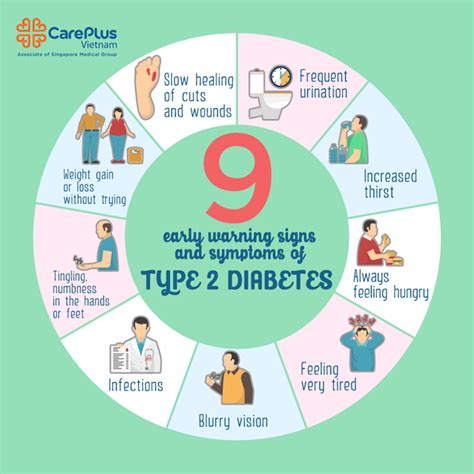
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Tingling or numbness in the hands and feet
- Recurring skin, gum, or bladder infections
Diagnosis of Type 2 Diabetes
Diagnosing type 2 diabetes typically involves a combination of physical examination, medical history, and laboratory tests. The most common tests used to diagnose type 2 diabetes include:- Fasting plasma glucose (FPG) test: This test measures blood glucose levels after an overnight fast.
- Oral glucose tolerance test (OGTT): This test measures blood glucose levels after consuming a sugary drink.
- Hemoglobin A1c (HbA1c) test: This test measures average blood glucose levels over the past 2-3 months.
Treatment and Management of Type 2 Diabetes
- Healthy eating: Eating a balanced diet that is low in sugar, salt, and unhealthy fats, and high in fiber, fruits, and vegetables.
- Regular physical activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, per week.
- Weight loss: Losing weight, particularly around the abdominal area, can help to improve insulin sensitivity and reduce the risk of complications.
- Stress management: Engaging in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can help to manage stress and improve overall well-being.
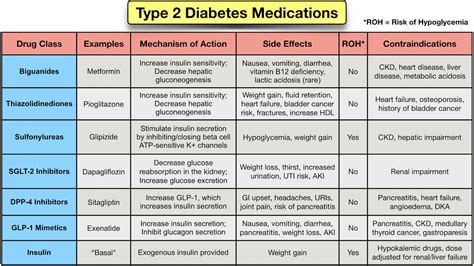
Medications may include:
- Metformin: A medication that helps to improve insulin sensitivity and reduce glucose production in the liver.
- Sulfonylureas: Medications that stimulate the pancreas to produce more insulin.
- Meglitinides: Medications that stimulate the pancreas to produce more insulin.
- Thiazolidinediones: Medications that help to improve insulin sensitivity.
- SGLT2 inhibitors: Medications that help to reduce glucose reabsorption in the kidneys.
Complications of Type 2 Diabetes
If left untreated or poorly managed, type 2 diabetes can lead to a range of serious complications, including:- Heart disease: High blood pressure and high cholesterol can increase the risk of heart disease, including heart attacks, strokes, and peripheral artery disease.
- Kidney damage: High blood sugar levels can damage the kidneys, leading to kidney failure and the need for dialysis or a kidney transplant.
- Nerve damage: High blood sugar levels can damage the nerves, leading to numbness, tingling, and pain in the hands and feet.
- Blindness: High blood sugar levels can damage the blood vessels in the eyes, leading to blindness.
- Amputations: Nerve damage and poor circulation can increase the risk of amputations, particularly in the feet.
Prevention of Type 2 Diabetes
- Maintaining a healthy weight: Losing weight, particularly around the abdominal area, can help to improve insulin sensitivity and reduce the risk of type 2 diabetes.
- Engaging in regular physical activity: Regular physical activity can help to improve insulin sensitivity and reduce the risk of type 2 diabetes.
- Eating a healthy diet: Eating a balanced diet that is low in sugar, salt, and unhealthy fats, and high in fiber, fruits, and vegetables, can help to reduce the risk of type 2 diabetes.
- Managing stress: Engaging in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can help to manage stress and improve overall well-being.
Early Intervention
Early intervention is critical in preventing type 2 diabetes. This may involve:- Screening for prediabetes: Screening for prediabetes, a condition characterized by high blood sugar levels that are not high enough to be classified as diabetes, can help to identify individuals at risk of developing type 2 diabetes.
- Lifestyle modifications: Implementing lifestyle modifications, such as healthy eating and regular physical activity, can help to improve insulin sensitivity and reduce the risk of type 2 diabetes.
- Medications: In some cases, medications, such as metformin, may be prescribed to help prevent type 2 diabetes in individuals at high risk.
What are the symptoms of type 2 diabetes?
+The symptoms of type 2 diabetes can be subtle and may develop gradually over time. Common symptoms include increased thirst and urination, fatigue, blurred vision, slow healing of cuts and wounds, tingling or numbness in the hands and feet, and recurring skin, gum, or bladder infections.
How is type 2 diabetes diagnosed?
+Diagnosing type 2 diabetes typically involves a combination of physical examination, medical history, and laboratory tests. The most common tests used to diagnose type 2 diabetes include fasting plasma glucose (FPG) test, oral glucose tolerance test (OGTT), and hemoglobin A1c (HbA1c) test.
Can type 2 diabetes be prevented?
+Yes, preventing type 2 diabetes is possible through a combination of lifestyle modifications and early intervention. Key strategies include maintaining a healthy weight, engaging in regular physical activity, eating a healthy diet, and managing stress.
In conclusion, type 2 diabetes is a complex and multifaceted condition that requires a comprehensive approach to management and prevention. By understanding the causes, symptoms, diagnosis, treatment options, and management strategies, individuals can take control of their health and reduce their risk of developing type 2 diabetes. We invite you to share your thoughts and experiences with type 2 diabetes in the comments below, and to share this article with anyone who may be affected by this condition. Together, we can work towards a healthier and more informed community.
