Intro
Identify Gerd symptoms in infants, including reflux, vomiting, and feeding issues. Learn about acid reflux, digestive problems, and infant care.
Gastroesophageal reflux disease, commonly referred to as GERD, is a condition where stomach acid frequently flows back into the tube connecting the mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of the esophagus, causing discomfort. While GERD can affect anyone, it's particularly common in infants. In fact, more than half of all babies experience some form of reflux during their first three months. Understanding the symptoms of GERD in infants is crucial for parents and caregivers to provide the necessary care and seek medical attention when needed.
Infant GERD symptoms can be subtle and may resemble those of other conditions, making diagnosis challenging. However, being aware of the common signs can help in early detection and management. Some of the typical symptoms include spitting up or vomiting, especially after feeding, though this is also a common occurrence in healthy infants. Other signs might include arching of the back, fussiness or irritability, especially after eating, and refusal to feed due to discomfort. In more severe cases, infants might experience difficulty gaining weight, coughing, or wheezing, and in rare instances, they might have signs of blood in their stool or vomit.
The importance of recognizing these symptoms lies in the potential for complications if left untreated. GERD can lead to feeding problems, poor growth, and an increased risk of respiratory issues due to the aspiration of stomach contents into the lungs. Furthermore, chronic exposure to stomach acid can cause esophagitis, an inflammation of the esophagus, leading to pain and difficulty swallowing. Given these potential complications, it's essential for parents to be vigilant and consult with their pediatrician if they suspect their infant is experiencing GERD symptoms. The pediatrician can provide guidance on managing symptoms, suggest lifestyle changes, and recommend further testing if necessary to confirm the diagnosis and rule out other conditions.
Understanding GERD in Infants

Understanding GERD in infants begins with recognizing that the condition is quite common and usually resolves on its own by the time the baby is 12 to 18 months old. The lower esophageal sphincter (LES), which is a ring-like muscle that separates the esophagus and stomach, is not fully developed in infants. This underdevelopment can cause the LES to open frequently, allowing stomach acid to flow back up into the esophagus. Additionally, infants spend a lot of time lying down, which can exacerbate reflux, and their diets are primarily liquid, making it easier for stomach contents to flow back up into the esophagus.
Causes and Risk Factors

Several factors can increase an infant's risk of developing GERD. Premature babies are at a higher risk due to their underdeveloped digestive systems. Similarly, babies with a low birth weight may experience GERD more frequently. Other risk factors include a family history of GERD, allergies, or sensitivities to milk or other foods, which can exacerbate symptoms. In some cases, structural abnormalities, such as pyloric stenosis or esophageal dysmotility, can also contribute to the development of GERD.
Diagnosing GERD in Infants

Diagnosing GERD in infants typically begins with a physical examination and a thorough medical history. The pediatrician will look for signs of poor growth, respiratory issues, or other complications. In many cases, a diagnosis can be made based on the infant's symptoms and how they respond to feeding changes or other initial treatments. However, if the symptoms are severe or do not improve with initial management, further testing may be recommended. This can include an upper GI series (a type of X-ray), endoscopy (to visually examine the esophagus and stomach), or pH monitoring (to measure the acidity in the esophagus).
Treatment and Management
Treatment for GERD in infants usually involves lifestyle changes and, in some cases, medication. Lifestyle modifications can include feeding smaller, more frequent meals to reduce the amount of food in the stomach, burping the baby more frequently during feedings, keeping the baby upright for 30 minutes after feeding, and elevating the head of the baby's bed by about 30 degrees. For breastfed babies, mothers may be advised to eliminate dairy products or other potential allergens from their diet to see if symptoms improve. Formula-fed babies might be switched to a hypoallergenic formula.
Medications for Infant GERD

In cases where lifestyle changes are not sufficient to manage symptoms, medications may be prescribed. The most common medications for infant GERD are antacids, which help neutralize stomach acid, and acid reducers or proton pump inhibitors, which decrease the amount of acid the stomach produces. However, medication should only be used under the guidance of a pediatrician, as there are potential side effects and long-term risks associated with their use in infants.
Home Remedies and Dietary Changes

Several home remedies and dietary changes can help alleviate GERD symptoms in infants. Keeping the infant upright after feedings can help prevent stomach acid from flowing back into the esophagus. Thickening feeds with a small amount of oatmeal cereal (for formula-fed babies) can also help reduce spit-up. For breastfed babies, ensuring a good latch can help reduce air swallowing during feeding, which may contribute to reflux. Additionally, avoiding overfeeding and introducing solid foods at an appropriate age can help manage symptoms.
Complications of Untreated GERD
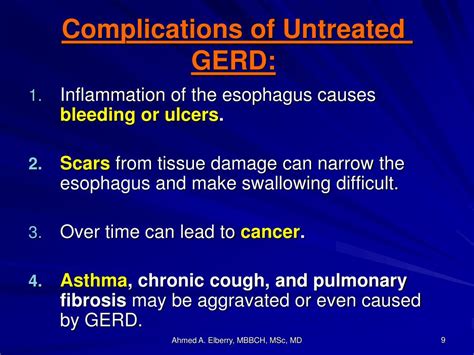
If left untreated, GERD can lead to several complications in infants. One of the most common complications is esophagitis, an inflammation of the esophagus that can cause pain and difficulty swallowing. Infants with GERD are also at an increased risk of respiratory problems, such as aspiration pneumonia, where stomach contents are inhaled into the lungs. Furthermore, chronic reflux can lead to narrowing of the esophagus (stricture), making swallowing difficult. In severe cases, untreated GERD can lead to failure to thrive due to inadequate nutrition and significant weight loss.
Prevention Strategies

While it may not be possible to completely prevent GERD in infants, certain strategies can reduce the risk or alleviate symptoms. For example, breastfeeding has been shown to reduce the risk of GERD, as breast milk is less likely to cause allergies or irritate the stomach compared to formula. Avoiding tobacco smoke, which can relax the lower esophageal sphincter and worsen reflux, is also crucial. Ensuring the infant is at a healthy weight and avoiding overfeeding can also help manage symptoms.
Support for Parents and Caregivers

Managing an infant with GERD can be challenging and stressful for parents and caregivers. It's essential to remember that the condition is common and, in most cases, temporary. Reaching out to healthcare providers, support groups, or online communities can provide valuable advice, emotional support, and reassurance. Sharing experiences and tips with others who are going through similar situations can be incredibly helpful. Additionally, taking care of one's own physical and mental health is vital to ensure the ability to provide the best possible care for the infant.
Future Outlook

The future outlook for infants with GERD is generally positive. Most babies outgrow the condition by the time they are 12 to 18 months old, as the lower esophageal sphincter matures and becomes more effective at preventing stomach acid from entering the esophagus. For some infants, however, GERD may persist into childhood or even adulthood, requiring ongoing management and treatment. Advances in medical research and treatment options continue to improve the management of GERD, offering hope for more effective and less invasive treatments in the future.
What are the most common symptoms of GERD in infants?
+The most common symptoms include spitting up or vomiting, arching of the back, fussiness or irritability, especially after eating, and refusal to feed due to discomfort.
How is GERD diagnosed in infants?
+Diagnosis typically begins with a physical examination and a thorough medical history. Further testing, such as an upper GI series, endoscopy, or pH monitoring, may be recommended if symptoms are severe or do not improve with initial management.
What are the potential complications of untreated GERD in infants?
+Potential complications include esophagitis, respiratory problems such as aspiration pneumonia, narrowing of the esophagus (stricture), and failure to thrive due to inadequate nutrition and significant weight loss.
In conclusion, while GERD can be a challenging condition for infants and their caregivers, understanding its symptoms, causes, and management strategies can significantly improve the quality of life for affected families. By recognizing the signs of GERD, seeking medical advice when necessary, and implementing appropriate lifestyle changes and treatments, parents and caregivers can help their infants navigate this condition and reduce the risk of complications. As research continues to uncover more about GERD and its effects on infants, there is hope for even more effective treatments and management options in the future. We invite readers to share their experiences, ask questions, and seek support from healthcare professionals and communities to ensure the best possible care for infants with GERD.
