Intro
The importance of respiratory health cannot be overstated, as it directly affects an individual's overall well-being and quality of life. One crucial tool used to assess and improve lung function is the incentive spirometer. This device is designed to help patients understand their breathing capabilities and work towards enhancing their lung capacity. By providing a visual incentive, it encourages users to take deep, sustained breaths, thereby strengthening their respiratory muscles and improving gas exchange. Understanding the normal range for an incentive spirometer is essential for both healthcare professionals and patients to set realistic goals and track progress effectively.
Respiratory health is a critical aspect of medical care, especially for individuals recovering from surgery, suffering from respiratory conditions like chronic obstructive pulmonary disease (COPD), or experiencing any form of lung impairment. The incentive spirometer plays a pivotal role in the management and rehabilitation of such conditions by offering a straightforward, yet effective method to monitor and improve lung function. It measures the volume of air inhaled and exhaled by the lungs, providing vital information on the patient's respiratory status. This information is not only useful for diagnosing respiratory issues but also for tailoring treatment plans to meet the specific needs of each patient.
The use of incentive spirometers has become increasingly popular due to their simplicity and effectiveness. They are widely used in hospitals, clinics, and even at home, making respiratory therapy more accessible and convenient for patients. By setting goals based on the normal range of lung function, patients are motivated to adhere to their treatment plans, leading to better outcomes and faster recovery times. Moreover, understanding the normal range helps in early detection of any deviations from healthy lung function, allowing for prompt intervention and preventing potential complications. This proactive approach to respiratory health underscores the significance of familiarizing oneself with the normal range of incentive spirometer readings.
Incentive Spirometer Basics
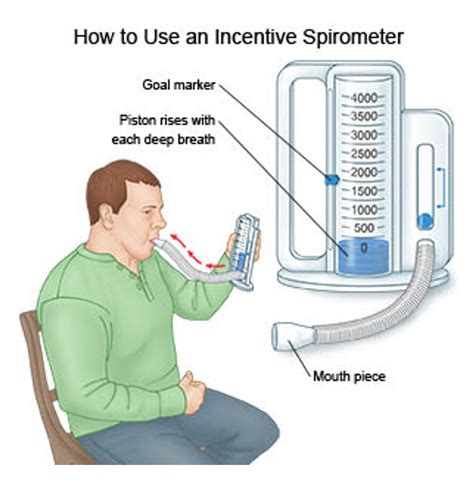
To grasp the concept of a normal range, it's essential to understand how an incentive spirometer works. This device typically consists of a tube connected to a chamber that contains a movable indicator. When a patient inhales through the tube, the indicator rises in proportion to the volume of air inhaled. The goal is to inhale deeply enough to move the indicator to a predetermined level, which is often set based on the patient's previous best effort or a target volume. This visual feedback serves as a powerful incentive for patients to strive for deeper, more effective breaths, thus aiding in the recovery and strengthening of lung function.
Normal Range for Incentive Spirometer
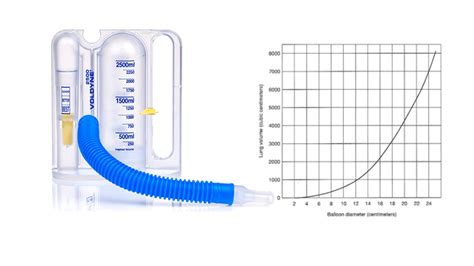
The normal range for an incentive spirometer can vary depending on several factors, including age, sex, height, and overall health of the patient. Generally, a healthy adult is expected to achieve a certain level of lung volume, typically measured in liters. For instance, the normal range for a forced vital capacity (FVC), which is the amount of air that can be forcibly exhaled after a maximal inspiration, is usually between 3 to 5 liters for adults, with variations based on individual characteristics. Understanding these ranges is crucial for setting realistic goals and evaluating the effectiveness of respiratory therapy.
Factors Influencing Normal Range
Several factors can influence what is considered a normal range for an incentive spirometer. These include:
- Age: Lung function tends to decrease with age, so older adults may have a lower normal range compared to younger individuals.
- Sex: On average, men tend to have larger lung capacities than women due to differences in body size and muscle mass.
- Height: Taller individuals typically have larger lung volumes, as there is a correlation between height and lung capacity.
- Overall Health: Presence of respiratory or other health conditions can significantly impact lung function and the normal range for an individual.
Benefits of Using Incentive Spirometers
The benefits of incorporating incentive spirometers into respiratory care are multifaceted. They not only provide a clear, measurable goal for patients to work towards but also offer a sense of achievement and motivation as progress is made. This positive reinforcement can lead to increased adherence to treatment plans, faster recovery from respiratory issues, and improved overall lung health. Furthermore, the use of incentive spirometers can help in the early detection of respiratory problems, facilitating timely interventions and potentially reducing the risk of complications.
Practical Applications
In practical terms, incentive spirometers are used in a variety of settings, including:
- Post-Surgical Care: To help patients recover lung function after surgery, especially after procedures that affect the lungs or require general anesthesia.
- Respiratory Therapy: For patients with chronic respiratory conditions, such as COPD or asthma, to improve lung function and manage symptoms.
- Home Care: Patients can use incentive spirometers at home under the guidance of healthcare professionals to continue their respiratory therapy and monitor their progress.
Steps to Improve Lung Function with Incentive Spirometers

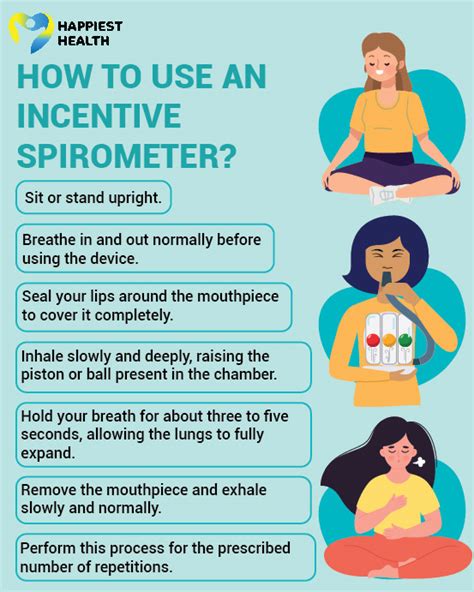
Improving lung function with an incentive spirometer involves a consistent and patient-centered approach. Here are key steps:
- Set Realistic Goals: Based on the patient's current lung function and health status, set achievable targets for incentive spirometer readings.
- Regular Practice: Encourage patients to use the incentive spirometer regularly, ideally several times a day, to practice deep breathing exercises.
- Monitor Progress: Regularly assess the patient's progress, adjusting goals as necessary to ensure continued motivation and improvement.
- Combine with Other Therapies: Incentive spirometry can be more effective when used in conjunction with other respiratory therapies and exercises.
Tips for Effective Use
- Proper Technique: Ensure that patients understand and use the correct technique when inhaling through the spirometer to get accurate readings.
- Consistency: Consistency is key; encourage patients to make incentive spirometer use a part of their daily routine.
- Feedback and Support: Provide regular feedback and support to patients, celebrating their successes and addressing any challenges they face.
Conclusion and Future Directions

In conclusion, understanding the normal range for an incentive spirometer is vital for effective respiratory therapy. By recognizing the factors that influence lung function and setting realistic, achievable goals, patients can work towards improving their respiratory health. As healthcare continues to evolve, the role of incentive spirometers is likely to expand, incorporating technology to provide more personalized and engaging respiratory therapy. The future of respiratory care may involve integrating incentive spirometers with digital platforms, offering remote monitoring capabilities, and developing more sophisticated algorithms to tailor therapy to individual patient needs.
Final Thoughts on Incentive Spirometers

As we look to the future, it's clear that incentive spirometers will remain a valuable tool in the management and rehabilitation of respiratory conditions. Their simplicity, effectiveness, and the motivation they provide to patients make them an indispensable part of respiratory therapy. Whether used in a clinical setting or at home, incentive spirometers offer a proactive approach to improving lung health, emphasizing the importance of patient engagement and empowerment in the healing process.
Call to Action

We invite you to share your experiences with incentive spirometers, whether as a healthcare professional or a patient. Your stories and insights can provide valuable encouragement and practical advice to others who are embarking on their journey to improve their respiratory health. Together, we can promote a better understanding of the importance of lung function and the role that incentive spirometers play in achieving healthier lungs and a better quality of life. Please feel free to comment below, and let's start a conversation about the impact of incentive spirometers on respiratory care.
What is the primary purpose of an incentive spirometer?
+The primary purpose of an incentive spirometer is to help patients improve their lung function by providing a visual incentive to take deep, sustained breaths, thereby strengthening their respiratory muscles and improving gas exchange.
How often should an incentive spirometer be used for effective respiratory therapy?
+For effective respiratory therapy, an incentive spirometer should be used several times a day, ideally at the same times each day, to practice deep breathing exercises and monitor progress consistently.
Can incentive spirometers be used by patients with chronic respiratory conditions at home?
+Yes, incentive spirometers can be used by patients with chronic respiratory conditions at home under the guidance of healthcare professionals. This allows for continued respiratory therapy and monitoring of lung function in a convenient and accessible manner.
