Intro
Discover the normal INR value range and understand its significance in blood clotting tests, including prothrombin time and international normalized ratio, to monitor health and prevent thrombosis risks.
The importance of understanding the International Normalized Ratio (INR) cannot be overstated, especially for individuals who are on anticoagulant therapy, such as warfarin. The INR is a test used to measure the time it takes for blood to clot and is primarily used to monitor patients on warfarin therapy, ensuring that their blood is within the therapeutic range - not too prone to clotting, which could lead to thrombosis, nor too prone to bleeding. This delicate balance is crucial for the management of conditions such as atrial fibrillation, deep vein thrombosis, and pulmonary embolism, among others. The INR normal value range is a critical piece of information for both healthcare providers and patients alike, as it guides the adjustment of anticoagulant doses to achieve optimal therapeutic effects while minimizing risks.
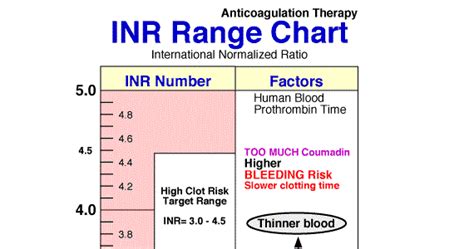
For individuals not on anticoagulant therapy, the normal INR range is typically between 0.9 and 1.1. This range indicates that the blood is clotting at a rate that is considered normal. However, for patients on warfarin or other anticoagulants, the target INR range varies depending on the condition being treated. For example, for patients with mechanical heart valves, the target INR range might be between 2.0 and 3.0, while for those with atrial fibrillation, the range is usually between 2.0 and 3.0 as well. Understanding these ranges is essential for managing anticoagulation therapy effectively and safely.
The INR test is a significant advancement in the field of coagulation studies, offering a standardized method to monitor the effects of anticoagulants. It has become an indispensable tool in clinical practice, allowing healthcare providers to tailor anticoagulant therapy to the individual needs of each patient. By maintaining the INR within the therapeutic range, healthcare providers can reduce the risk of thromboembolic events and minimize the risk of bleeding complications. As such, the INR normal value range, and more specifically, the therapeutic range for each condition, is a critical component of patient care for those on anticoagulant therapy.
Understanding INR Values
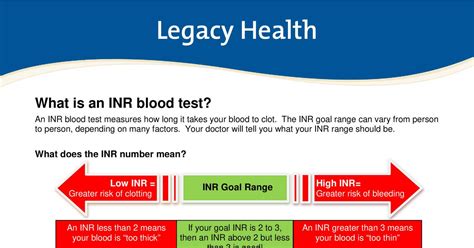
Understanding INR values is fundamental for both healthcare providers and patients. An INR value within the normal range for someone not on anticoagulants (0.9-1.1) indicates that the blood is clotting normally. However, for those on anticoagulant therapy, the goal is to maintain the INR within a specific therapeutic range. This range is condition-specific and is determined based on the balance between the risk of thrombosis and the risk of bleeding. For instance, an INR value of 2.5 for someone with atrial fibrillation might be considered within the therapeutic range, indicating that the anticoagulant is effectively reducing the risk of stroke without significantly increasing the risk of bleeding.
Interpreting INR Results
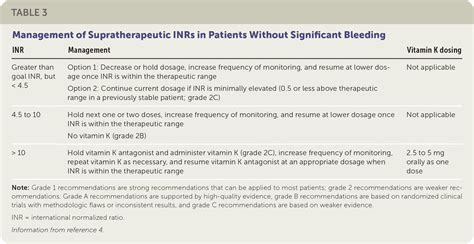
Interpreting INR results requires an understanding of the therapeutic range for the specific condition being treated. Results that fall within this range indicate that the patient's anticoagulation therapy is effective and at a safe level. Results below the therapeutic range may indicate an increased risk of thrombosis, suggesting the need for an increase in anticoagulant dosage. Conversely, results above the therapeutic range may signal an increased risk of bleeding, necessitating a reduction in dosage. Regular monitoring of INR levels is essential to adjust anticoagulant doses appropriately and to maintain the patient within the therapeutic range.Factors Influencing INR Values
Several factors can influence INR values, including diet, other medications, and certain medical conditions. Foods high in vitamin K, such as leafy green vegetables, can decrease INR values because vitamin K is essential for the production of clotting factors in the liver. Other medications, including antibiotics and anti-inflammatory drugs, can also affect INR levels by interacting with the anticoagulant. Certain medical conditions, like liver disease, can impact the liver's ability to produce clotting factors, thereby influencing INR results. Understanding these factors is crucial for managing anticoagulation therapy effectively and for interpreting INR results accurately.
Dietary Considerations
Dietary considerations play a significant role in managing INR values. Patients on warfarin are often advised to maintain a consistent intake of vitamin K-rich foods to avoid significant fluctuations in INR levels. Major changes in dietary habits, such as significantly increasing or decreasing consumption of foods high in vitamin K, should be discussed with a healthcare provider, as these changes can impact anticoagulation therapy. Additionally, cranberry juice and grapefruit juice are known to interact with warfarin, potentially altering INR levels. Therefore, patients should be cautious with the consumption of these juices while on anticoagulant therapy.Managing INR Values

Managing INR values effectively requires regular monitoring, adjustments to anticoagulant doses based on INR results, and careful consideration of factors that can influence INR levels. Patients should work closely with their healthcare providers to understand their target INR range and how to maintain it. This includes being aware of dietary restrictions, the potential interactions with other medications, and the importance of adhering to the prescribed anticoagulation regimen. Regular blood tests to check INR levels are essential, and the frequency of these tests can vary depending on the stability of the patient's INR results and the specific clinical scenario.
Challenges in INR Management
Despite the importance of maintaining INR values within the therapeutic range, several challenges exist in INR management. These include variability in patient response to anticoagulants, the potential for drug interactions, and the impact of dietary factors. Additionally, achieving and maintaining the therapeutic range can be challenging, especially in patients with conditions that affect the liver or kidneys, as these organs play critical roles in the metabolism and excretion of anticoagulants. Healthcare providers must be vigilant and proactive in addressing these challenges to ensure effective and safe anticoagulation therapy.Advancements in INR Monitoring
Advancements in INR monitoring have significantly improved the management of anticoagulation therapy. Point-of-care INR devices allow for rapid testing in clinical settings or even at home, enabling more frequent monitoring and quicker adjustments to anticoagulant doses. Additionally, the development of new anticoagulants with more predictable pharmacokinetics has reduced the need for frequent INR monitoring in some cases. These advancements have contributed to better outcomes for patients on anticoagulant therapy by reducing the risk of both thrombotic and bleeding complications.
Future Directions
Future directions in INR monitoring and anticoagulation therapy are focused on further personalizing treatment regimens and minimizing the risks associated with anticoagulant use. This includes the development of genetic tests to predict patient response to specific anticoagulants and the creation of novel anticoagulants with improved safety profiles. Moreover, the integration of technology, such as mobile health applications, can enhance patient engagement and adherence to anticoagulation therapy, potentially leading to better INR control and reduced complications.Conclusion and Next Steps

In conclusion, understanding the INR normal value range and the therapeutic ranges for specific conditions is crucial for the effective management of anticoagulation therapy. By recognizing the factors that influence INR values and staying informed about the latest advancements in INR monitoring and anticoagulant therapy, patients and healthcare providers can work together to minimize risks and maximize the benefits of anticoagulation. As research continues to evolve, it is essential to stay updated on the best practices for INR management and to embrace new technologies and therapies that can improve patient outcomes.

We invite you to share your thoughts and experiences with INR management and anticoagulation therapy. Your insights can help others better understand the complexities of managing INR values and the importance of personalized care in anticoagulant therapy. By engaging in this discussion, we can collectively contribute to improved patient outcomes and safer, more effective anticoagulation practices.
What is the normal INR range for someone not on anticoagulant therapy?
+The normal INR range for someone not on anticoagulant therapy is typically between 0.9 and 1.1.
How often should INR levels be checked for patients on warfarin?
+The frequency of INR checks for patients on warfarin can vary but is typically every 1-4 weeks, depending on the stability of the patient's INR results and the specific clinical scenario.
What foods can affect INR levels in patients on warfarin?
+Foods high in vitamin K, such as leafy green vegetables, can decrease INR levels. Additionally, cranberry and grapefruit juices are known to interact with warfarin and can affect INR levels.
