Intro
Discover rectal prolapse treatment options, including surgery, lifestyle changes, and physical therapy, to alleviate symptoms and improve bowel health, addressing related issues like fecal incontinence and rectal bleeding.
Rectal prolapse is a condition where the rectum loses its normal attachments inside the body, allowing it to protrude out through the anus. This condition can be extremely uncomfortable and may significantly impact an individual's quality of life. Understanding the available treatment options is crucial for managing rectal prolapse effectively. The importance of seeking medical attention cannot be overstated, as timely intervention can prevent further complications and improve outcomes.
The prevalence of rectal prolapse varies, but it is more common in older adults and individuals with a history of constipation, straining during bowel movements, or previous pelvic surgeries. Recognizing the signs and symptoms, such as a bulge or protrusion from the anus, rectal bleeding, or difficulty with bowel movements, is key to early diagnosis and treatment. The management of rectal prolapse involves a range of options, from lifestyle modifications and non-surgical treatments to surgical interventions, each tailored to the severity of the condition and the patient's overall health.
Rectal prolapse treatment has evolved significantly, offering patients a variety of choices that cater to their specific needs and preferences. From conservative management approaches aimed at alleviating symptoms to more invasive surgical procedures designed to correct the prolapse, the goal is to restore normal rectal function, alleviate discomfort, and improve the patient's quality of life. The decision on which treatment path to follow is made in consultation with healthcare providers, considering factors such as the degree of prolapse, the patient's age, health status, and personal preferences.
Understanding Rectal Prolapse

Causes and Risk Factors
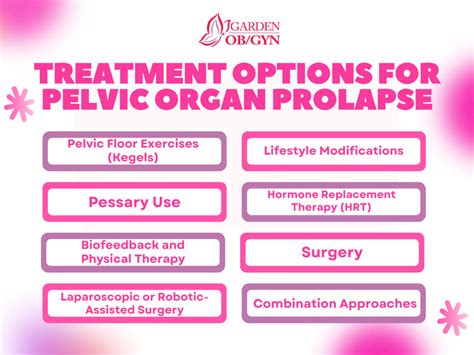
The causes of rectal prolapse are multifactorial and can include conditions that increase pressure on the rectum, such as chronic straining during bowel movements, or factors that weaken the pelvic floor muscles, such as childbirth or aging. Understanding these causes and identifying risk factors can help in the prevention and early detection of rectal prolapse. For instance, maintaining a healthy bowel habit, avoiding straining, and performing pelvic floor exercises (Kegel exercises) can reduce the risk of developing rectal prolapse.Treatment Options for Rectal Prolapse
Non-Surgical Management
Non-surgical management of rectal prolapse focuses on relieving symptoms and preventing further prolapse. This can include lifestyle modifications such as increasing fiber intake, drinking plenty of water, and exercising regularly. Biofeedback therapy may also be recommended to help patients become aware of and strengthen their pelvic floor muscles. For some patients, particularly those with significant co-morbidities or who are not candidates for surgery, non-surgical management may be the preferred approach.Surgical Treatment for Rectal Prolapse
Surgical Procedures
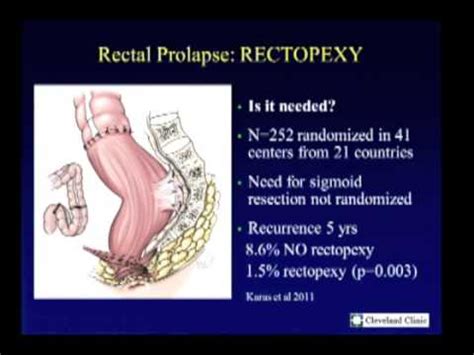
Surgical procedures for rectal prolapse can be broadly categorized into abdominal and perineal approaches. Abdominal approaches, such as rectopexy, involve attaching the rectum to the sacrum (the lower back portion of the pelvis) using mesh or sutures to lift it back into place. This can be done through open surgery or minimally invasive laparoscopic surgery. Perineal approaches, such as the Delorme procedure or perineal rectosigmoidectomy, are less invasive and may be preferred for older patients or those with significant medical conditions. These procedures involve removing a portion of the rectum or sigmoid colon through an incision in the perineum (the area between the anus and the vagina in women, or between the anus and the scrotum in men).Post-Surgical Care and Recovery

Preventing Recurrence
Preventing the recurrence of rectal prolapse involves a combination of lifestyle changes and, in some cases, ongoing medical management. Patients are advised to maintain a healthy diet rich in fiber, stay hydrated, and exercise regularly to prevent constipation. Pelvic floor exercises can help strengthen the muscles that support the rectum, reducing the risk of future prolapse. Regular follow-up with a healthcare provider is also important for early detection of any recurrence.Conclusion and Future Directions
Emerging Trends and Technologies
Emerging trends and technologies in the field of rectal prolapse treatment hold promise for even better outcomes. These include the use of robotic surgery for more precise and minimally invasive procedures, advancements in biomaterials for use in surgical mesh, and the integration of biofeedback and physical therapy into comprehensive treatment plans. As research continues to uncover the complexities of rectal prolapse, patients can expect more personalized and effective treatment options.What are the symptoms of rectal prolapse?
+The symptoms of rectal prolapse can include a bulge or protrusion from the anus, rectal bleeding, difficulty with bowel movements, and a feeling of incomplete evacuation. The severity of symptoms can vary depending on the degree of prolapse.
How is rectal prolapse diagnosed?
+Diagnosis of rectal prolapse typically involves a physical examination, where a healthcare provider may ask the patient to strain or cough to observe the prolapse. Additional tests such as colonoscopy, defecography, or MRI may be recommended to assess the extent of the prolapse and rule out other conditions.
Can rectal prolapse be prevented?
+While not all cases of rectal prolapse can be prevented, certain measures can reduce the risk. These include maintaining a healthy bowel habit, avoiding straining during bowel movements, performing pelvic floor exercises, and managing chronic conditions such as constipation or diarrhea.
What are the risks associated with surgical treatment for rectal prolapse?
+Risks associated with surgical treatment for rectal prolapse can include infection, bleeding, constipation, and recurrence of the prolapse. The choice of surgical procedure and the patient's overall health can influence the risk of complications.
How long does recovery take after surgery for rectal prolapse?
+Recovery time after surgery for rectal prolapse can vary depending on the type of surgery and the patient's health. Generally, patients can expect to spend several weeks recovering, with gradual return to normal activities over a few months. Follow-up care with a healthcare provider is crucial to ensure proper healing and to address any concerns.
We invite readers to share their experiences or ask questions about rectal prolapse treatment options in the comments below. For those seeking more information or support, there are numerous resources available, including patient advocacy groups and healthcare provider networks. By engaging in discussions and staying informed, we can work together to improve awareness and outcomes for individuals affected by rectal prolapse.
