Intro
Discover the potential side effects of Buprenorphine/Naloxone, including opioid withdrawal symptoms, addiction risks, and medication interactions, to ensure safe treatment and minimize adverse reactions.
The combination of buprenorphine and naloxone is a medication used to treat opioid addiction. Buprenorphine is a partial opioid agonist, which means it activates the opioid receptors in the brain but to a lesser extent than full agonists like heroin or methadone. Naloxone, on the other hand, is an opioid antagonist that can reverse the effects of an opioid overdose. When combined, buprenorphine and naloxone work together to help manage withdrawal symptoms and cravings in individuals trying to quit opioids. Despite its effectiveness, the use of buprenorphine/naloxone can lead to several side effects, which will be explored in this article.
The importance of understanding the side effects of buprenorphine/naloxone cannot be overstated. As with any medication, being aware of the potential risks and benefits is crucial for patients, healthcare providers, and loved ones. This knowledge enables informed decision-making and ensures that treatment is both safe and effective. Furthermore, recognizing the side effects can help in managing them, thereby improving the overall quality of life for individuals undergoing treatment for opioid addiction.
Opioid addiction is a serious condition that affects millions of people worldwide. The opioid crisis has led to a significant increase in overdose deaths, hospitalizations, and social and economic burdens on communities. Treatment options like buprenorphine/naloxone offer hope for recovery, but it's essential to approach these treatments with a comprehensive understanding of their implications. By delving into the side effects of buprenorphine/naloxone, we can better navigate the challenges of opioid addiction treatment and work towards more effective and compassionate care.
Introduction to Buprenorphine/Naloxone

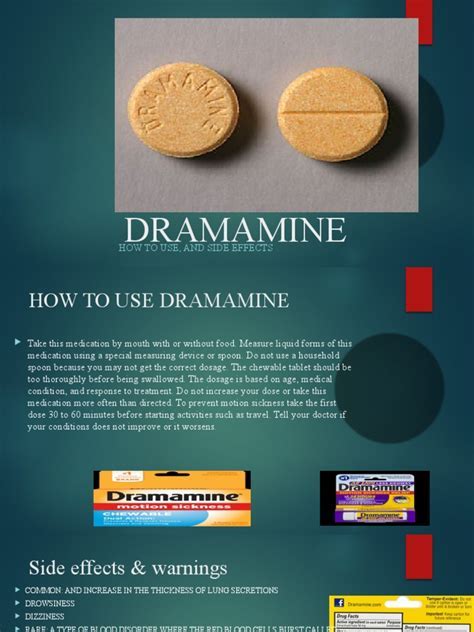
Buprenorphine/naloxone is administered sublingually (under the tongue) or as a buccal film (inside the cheek). The combination is designed to deter misuse; the naloxone component has minimal effect when taken as directed but can precipitate withdrawal if the medication is injected. This unique formulation helps reduce the risk of diversion and misuse, making it a safer option for treating opioid use disorder.
How Buprenorphine/Naloxone Works
The mechanism of action of buprenorphine/naloxone involves the partial activation of opioid receptors by buprenorphine, which helps to reduce cravings and withdrawal symptoms without producing the intense euphoria associated with full opioid agonists. Naloxone, being an antagonist, blocks the effects of opioids at their receptor sites, further reducing the potential for misuse. This dual-action approach makes buprenorphine/naloxone an effective tool in the management of opioid dependence.Common Side Effects of Buprenorphine/Naloxone

The side effects of buprenorphine/naloxone can vary from person to person. Common side effects include:
- Nausea and vomiting
- Headache
- Dizziness or lightheadedness
- Constipation
- Sleep disturbances
- Sweating
- Decreased appetite
These side effects are typically mild to moderate and may diminish over time as the body adjusts to the medication. However, it's crucial for patients to report any side effects to their healthcare provider to ensure safe and effective treatment.
Less Common but Serious Side Effects
While less common, there are more serious side effects associated with buprenorphine/naloxone that require immediate medical attention. These include: - Respiratory depression: Especially when combined with other central nervous system depressants like alcohol, benzodiazepines, or other opioids. - Allergic reactions: Symptoms can include rash, itching, swelling, severe dizziness, and trouble breathing. - Adrenal insufficiency: A condition where the adrenal glands do not produce adequate amounts of certain hormones. - Decreased liver function: Buprenorphine/naloxone should be used with caution in patients with pre-existing liver conditions.Managing Side Effects
Effective management of side effects is key to ensuring that patients can continue their treatment for opioid addiction without undue discomfort or risk. Strategies for managing side effects include:
- Dose adjustment: The healthcare provider may adjust the dose to minimize side effects while maintaining therapeutic efficacy.
- Symptomatic treatment: For example, anti-emetics for nausea, laxatives for constipation, and pain relievers for headache.
- Lifestyle modifications: Including dietary changes, regular exercise, and adequate sleep to help mitigate side effects like constipation and sleep disturbances.
Special Considerations
Certain populations, such as pregnant women, individuals with liver or kidney disease, and the elderly, may require special consideration when being treated with buprenorphine/naloxone. The risk-benefit analysis may differ for these groups, and dose adjustments or closer monitoring may be necessary.Long-Term Use and Withdrawal
Buprenorphine/naloxone is intended for long-term use as part of a comprehensive treatment plan for opioid addiction. However, like other opioids, physical dependence can develop. If the decision is made to discontinue treatment, it should be done under medical supervision to minimize withdrawal symptoms. Gradual tapering of the dose can help reduce the severity of withdrawal.
Tapering and Withdrawal Symptoms
Withdrawal symptoms from buprenorphine/naloxone can include: - Anxiety - Insomnia - Restlessness - Muscle and bone pain - Nausea and vomiting - Diarrhea - Abdominal crampsA slow and medically supervised taper can help alleviate these symptoms and make the transition off the medication more manageable.
Conclusion and Future Directions

In conclusion, while buprenorphine/naloxone is a valuable medication in the treatment of opioid addiction, it's essential to be aware of its potential side effects. By understanding these effects and how to manage them, patients and healthcare providers can work together to ensure safe and effective treatment. Future research should continue to explore ways to minimize side effects, improve treatment outcomes, and expand access to care for those affected by opioid addiction.
Final Thoughts
As we move forward in the fight against opioid addiction, medications like buprenorphine/naloxone will play a critical role. It's our responsibility to use these tools wisely, with a deep understanding of their benefits and risks. By doing so, we can offer hope and healing to those struggling with addiction and work towards a brighter, healthier future for all.What is the primary use of buprenorphine/naloxone?
+Buprenorphine/naloxone is primarily used to treat opioid addiction by managing withdrawal symptoms and reducing cravings.
Can buprenorphine/naloxone be used during pregnancy?
+Buprenorphine/naloxone can be used during pregnancy if the benefits outweigh the risks, but it should be done under close medical supervision.
How long does it take to feel the effects of buprenorphine/naloxone?
+The effects of buprenorphine/naloxone can be felt within 30 minutes to an hour after administration, with peak effects occurring a few hours later.
We invite you to share your thoughts and experiences with buprenorphine/naloxone in the comments below. Your insights can help others understand the complexities of opioid addiction treatment and the role that medications like buprenorphine/naloxone play in the recovery process. Let's work together to foster a supportive community that encourages open discussion and seeks solutions to the challenges posed by opioid addiction.
